Answer of May 2010
Clinical History:
A 15 years-old girl was presented with progressive lower limb weakness for 1 week. The lower limb weakness was preceded by repeated vomiting for few days. On physical examination, there was diminished deep tendon reflex of bilateral lower limbs. Bilateral lower limb power was 4/5. She was afebrile and not septic. CSF analysis revealed elevated CSF protein level with normal cell count and negative gram staining. An urgent MRI brain and whole spine was performed. Selected images of the MRI lumbar spine were illustrated.
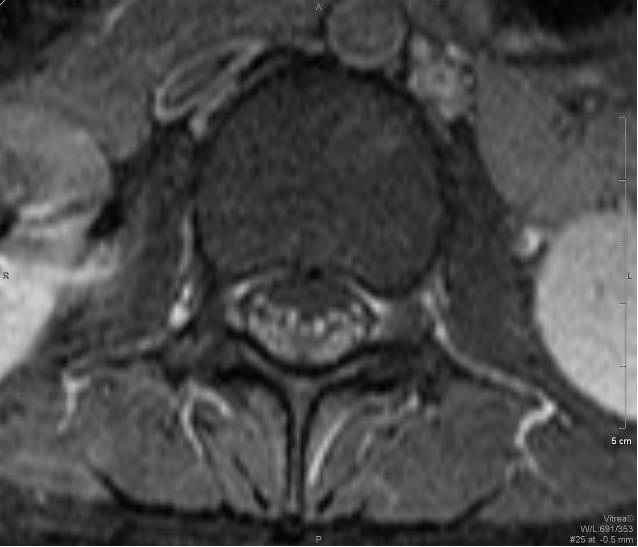
Fig. 1 T1 Axial Fig. 2 T2 Axial
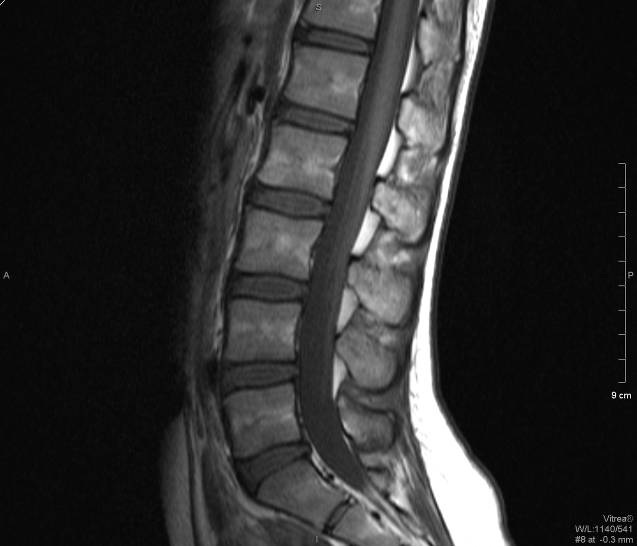
Fig. 3 T1+C FS Axial Fig. 4 T1 Sagittal
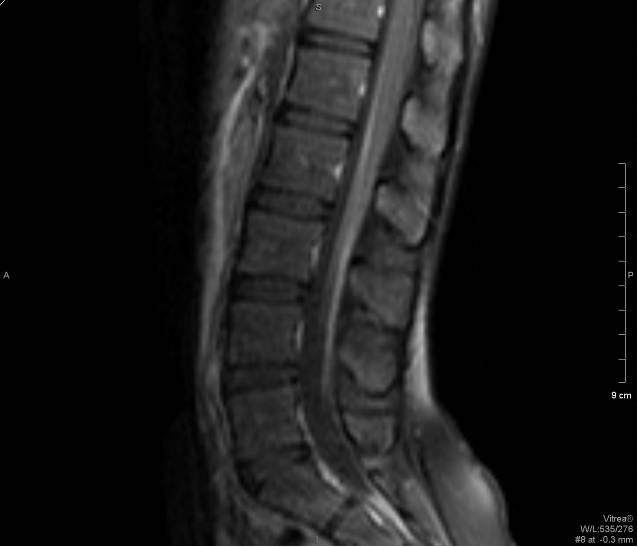
Fig. 5 T2 Sagittal Fig. 6 T1+C FS Sagittal
Diagnosis:
Guillain-Barre Syndrome
Discussion:
MRI of the lumbar spine shows marked enhancement of the cauda equina and pial surface of conus medullaris.
Guillain-Barre Syndrome (GBS), also called acute inflammatory demyelinating polyradiculoneuropathy (AIDP), is characterized by an acute monophasic, non-febrile, post-infectious illness manifesting as ascending weakness and areflexia.
Antecedent event or trigger can be identified in about 70% of patients. Usual triggers include antecedent gastrointestinal or respiratory tract infection. Campylobacter jejuni infection probably represents the most common trigger for the syndrome. Other triggering infectious agents include Epstein-Barr virus, cytomegalovirus, enteroviruses, hepatitis A and B, varicella and Mycoplasma pneumonia. A link to vaccination has been found with influenza vaccination with incidence of postinfluenza vaccination GBS approximately 0.75 per 1 million vaccinations.
Patient classically presents with bilateral symmetrical ascending paralysis. Ascend up to the brainstem may involve cranial nerves. Facial nerve is the most commonly involved cranial nerve and may be involved in up to 50% of cases. Areflexia is a classical and common finding in patient with GBS. Typical cerebrospinal fluid (CSF) finding in GBS would be albuminocytologic dissociation (ie. elevation of CSF protein with normal CSF cell count).
The MRI features of GBS include thickened nerve roots in T2 weighed images. There would be avid contrast enhancement of the cauda equina and pial surface of conus medullaris seen in post-gadolinium T1 weighed images. The ventral nerve roots are more commonly affected than the dorsal nerve roots.
Diagnosis of GBS relies on typical clinical features and is supported by the CSF analysis, MRI findings and electrodiagnostic studies.
Treatment for GBS has been aimed primarily at immunomodulation with the use of intravenous immunoglobulin (IVIG) or plasma exchange. There is no proven benefit from corticosteroid administration. Intensive care management would be needed in severe cases.