Answer of June 2010
Clinical History:
An 83-year old lady with good past health presents with congestive heart failure symptoms, complaining of dyspnoea, orthopnoea and ankle oedema since three days ago. Routine blood tests find deranged liver function (bili 37, ALT 22, ALP 288) and clotting profile (INR 1.5).
Diagnosis:
Acute Budd-Chiari Syndrome
Discussion:
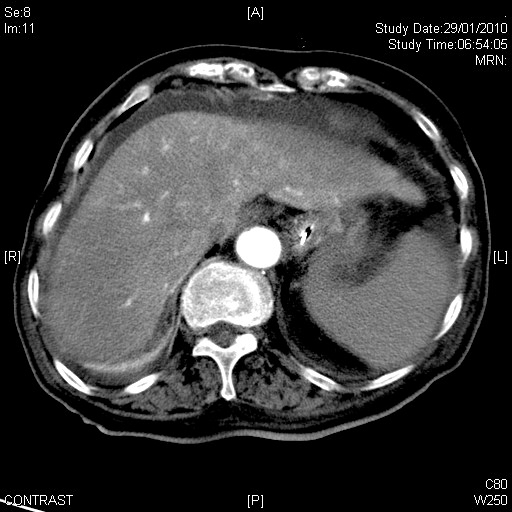
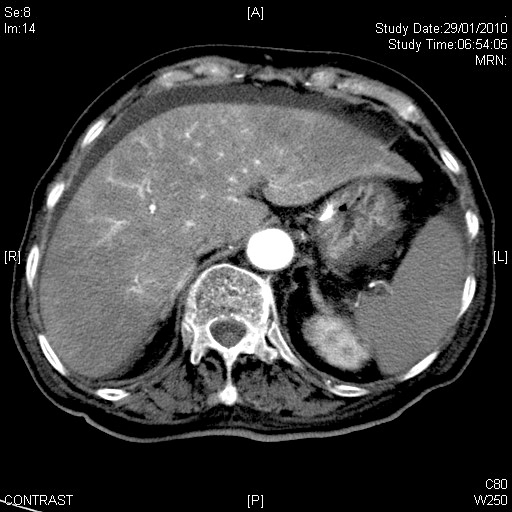
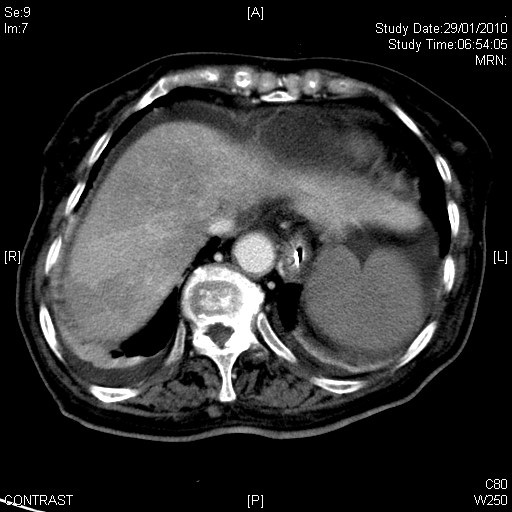
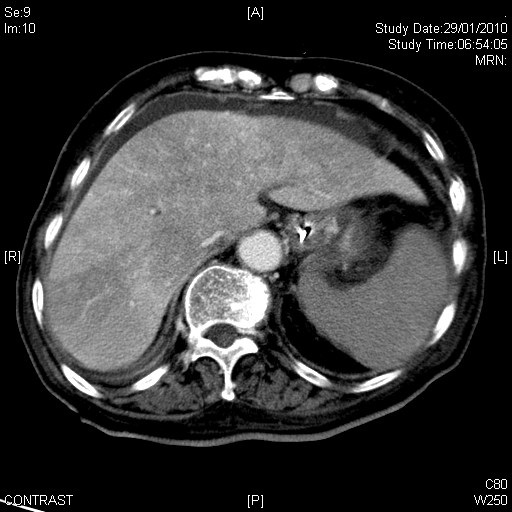
Dual-phase computed tomography shows heterogeneous hepatic parenchymal enhancement giving a "nutmeg-like" appearance, with a mild degree of periportal oedema. The hepatic veins are non-opacified and remain hypoattenuating while the intrahepatic inferior vena cava is narrowed. There is also mild enlargement of the spleen and ascites suggesting portal hypertension.
Budd-Chiari Syndrome is a group of disorders characterised by hepatic venous outflow obstruction at the level of the hepatic veins, inferior vena cava or right atrium. In the western world, 75% patient's with this syndrome have an underlying thrombotic tendency, such as oral contraceptive use, pregnancy, myeloproliferative disorders, antiphospholipid syndrome, and paroxysmal nocturnal haemoglobinuria. Membraneous webs or malignant tumours obstructing the hepatic veins or inferior vena cava may lead to Budd-Chiari syndrome. This patient had none of the conditions listed above. Congestive heart failure is not an established cause of Budd-Chiari syndrome, although both can present similarly with ascites and lower limb oedema. Budd-Chiari syndrome has been reported to precipitate cardiac failure through superior extension of thrombosis into the right atrium.
Clinical features range from mild symptoms to fulminant acute liver failure to chronic disease, depending on the extent and acuteness of hepatic venous obstruction and adequacy of remaining venous outflow. In acute Budd-Chiari disease, there is diffuse enlargement and hypoattenuation of the liver indicating congestive oedema. There is also differential contrast enhancement, with the peripheral regions showing weaker enhancement and the central region (including the caudate lobe) which have less affected venous drainage showing stronger enhancement. In chronic Budd-Chiari syndrome, there is atrophy of the peripheral regions of the liver, and parenchymal oedema is replaced by cirrhosis which is often accompanied by regenerative nodules. The central region is often hypertrophied in these cases. Ascites is seen with both acute and chronic forms of Budd-Chiari syndrome.
Most cases of Budd-Chiari syndrome progress to hepatic failure and death unless obstruction to venous outflow is relieved. Mild cases may be managed with anticoagulation to arrest progression of venous thrombosis. More severe cases may require angioplasty or stenting of occluded hepatic veins, or the creation of a portosystemic shunt, all of which can be performed via a transjugular approach.