Answer of December 2011
Clinical History:
A 64 year old woman presented with nipple discharge.
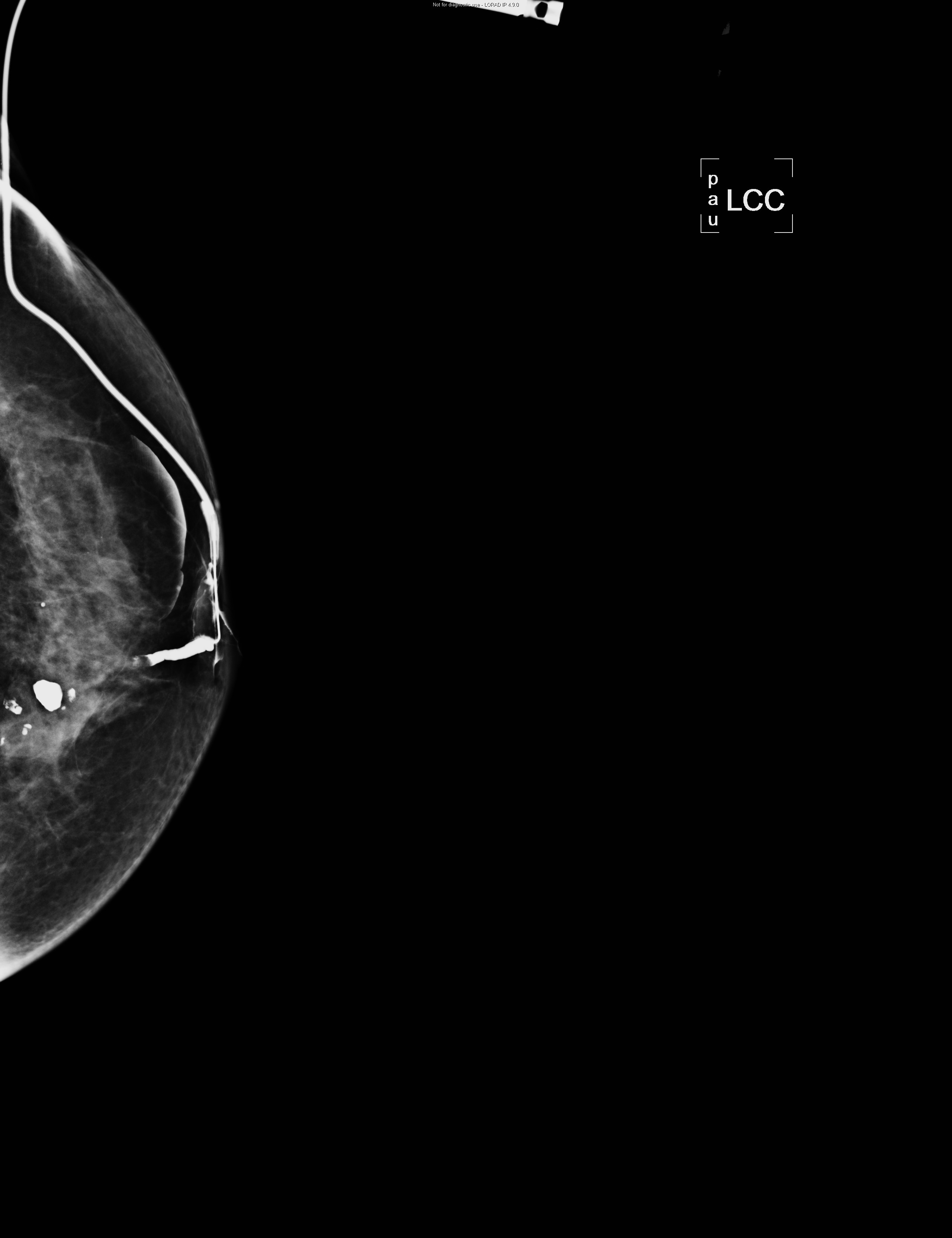
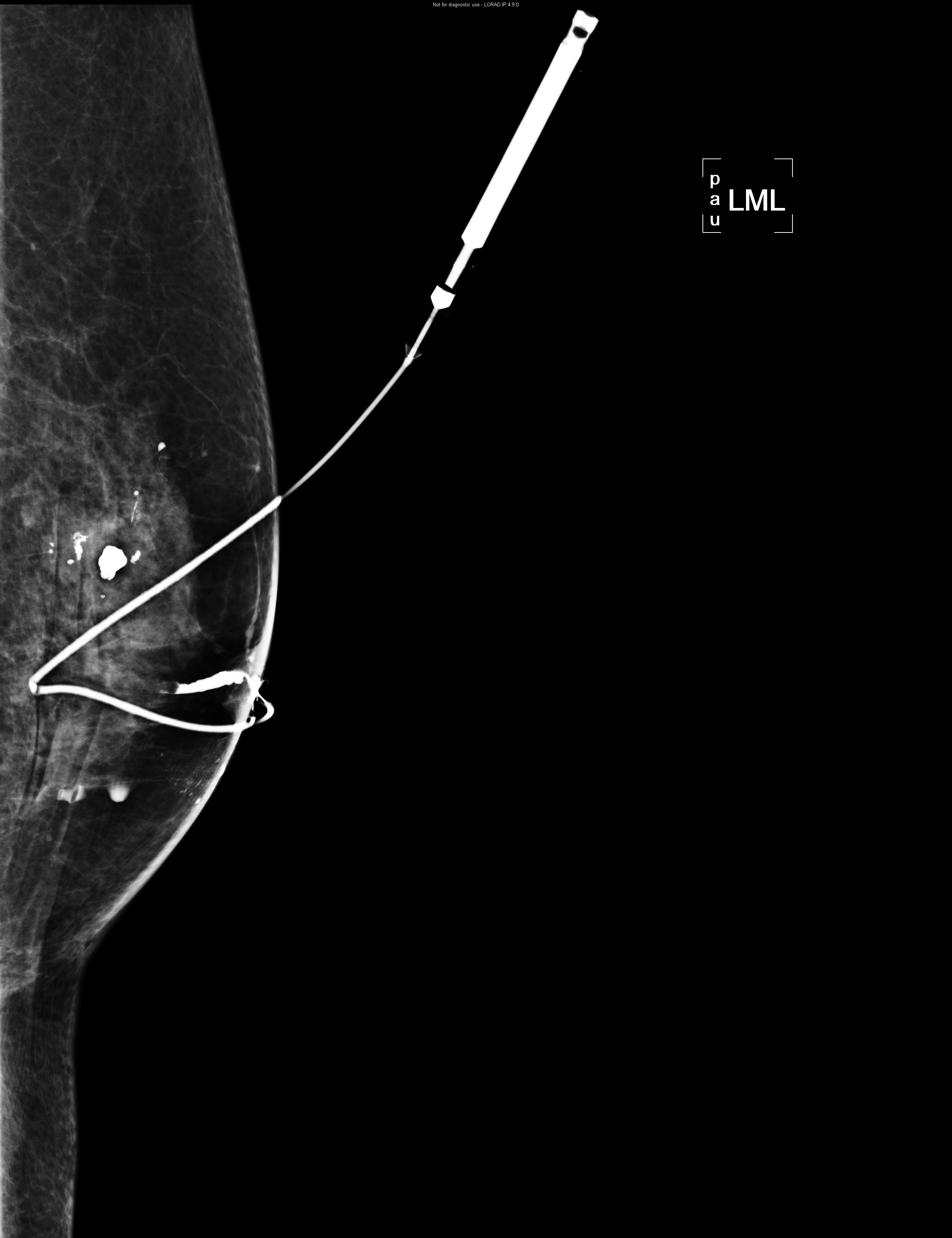
L ductogram (CC view) L ductogram (ML view)
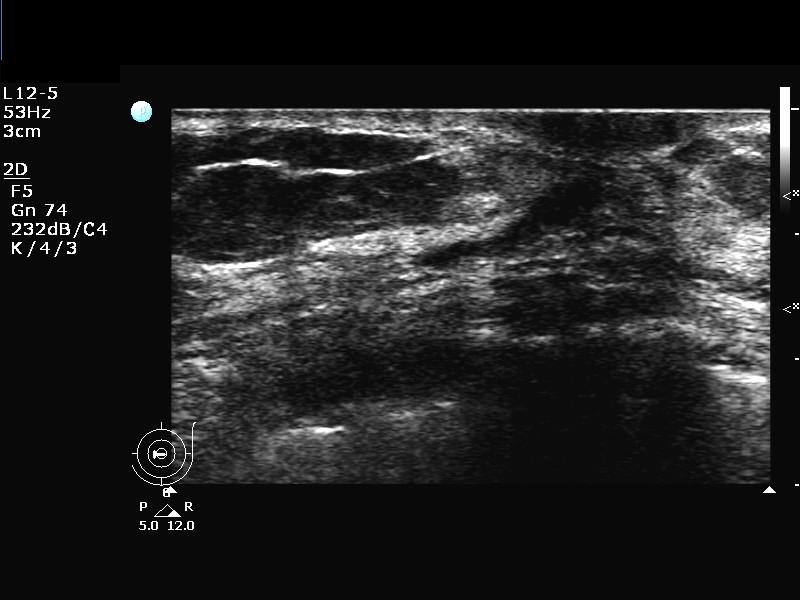
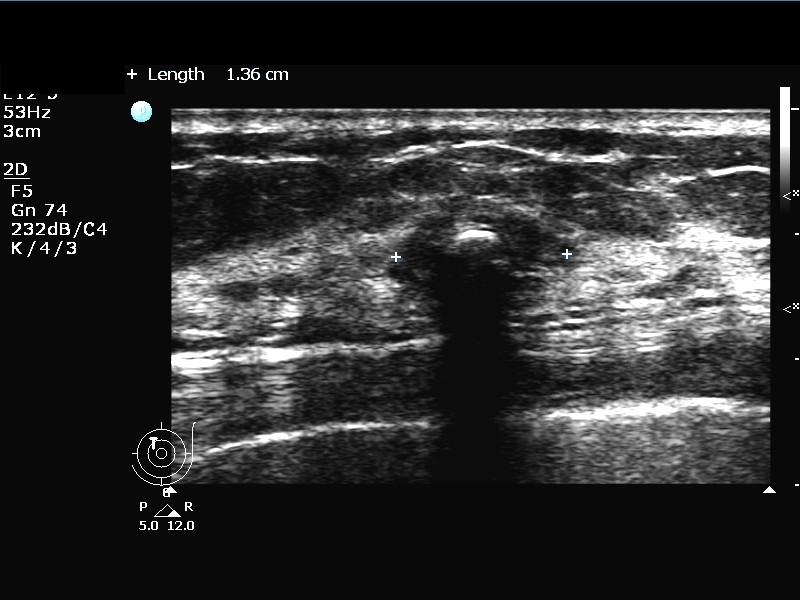
USG L9H USG L9H
USG L11H
Diagnosis:
Intraductal papilloma at L9H and fibroadenoma at L11H
Discussion:
Findings:
Ductogram -
A filling defect completely blocking the duct is noted slightly medial to nipple (L9H) and 1.5cm deep to the skin. It is 2mm thick. The proximal duct is not opacified and therefore its proximal extent cannot be delineated.
Popcorn calcifications are present at upper inner quadrant of left breast, suggestive of hyalinised fibroadenoma.
No suspicious microcalcification or architectural distortions are seen.
No enlarged axillary lymphadenopathy.
Fig 1. Left ductogram of L9H discharging duct (a) L CC (b) L ML showing an obstructing filling defect in dilated L9H duct. No opacification of proximal duct is observed.
USG -
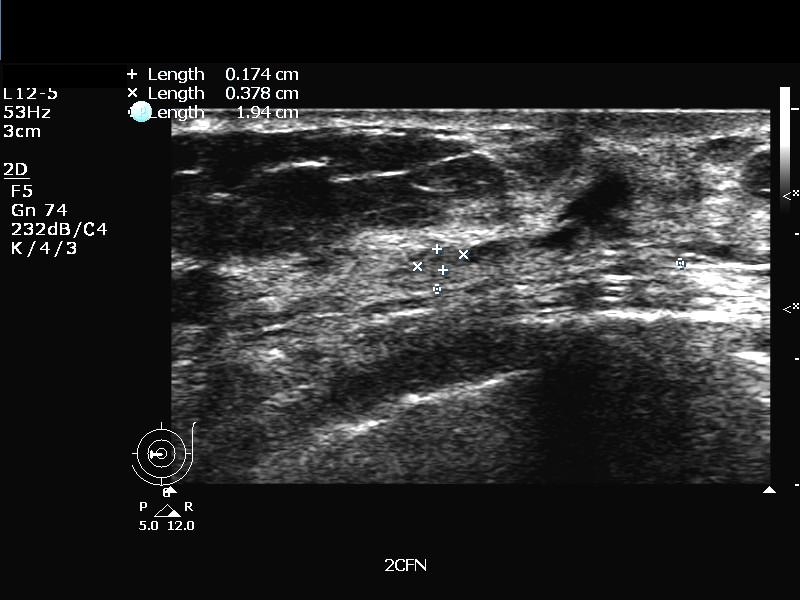
There is a fluid-distended duct at L9H extending medially for 2cm where a 1.7x3.7mm slightly hypoechoic nodule is seen within it, without increase in vascularity.
An ovoid hypoechoic lesion with macrocalcification is seen at L11H, measuring 2x0.8x1.4cm.
Fig 2. Ultrasound of the left breast shows (a) dilated duct at L9H, (b) intraductal nodule and (c) L11H hypoechoic mass with coarse calcification.
Further management:
The patient then underwent left ductoscopy and microdochetomy of the L9H discharge duct and excision of the L11H mass. Pathology shows intraductal papilloma at L9H and fibroadenoma at L11H.
Discussion:
Popcorn coarse calcification on mammogram is suggestive of benignity. It signifies calcific degenerative fibroadenoma. On ultrasound, fibroadenoma commonly present as ovoid hypoechoic lesion with circumscribed/ mildly lobulated border and sometimes coarse calcifications. These features were present in our patient’s L11H lesion which was confirmed to be fibroadenoma on histology.
The primary indication for ductography is spontaneous, unilateral, single duct nipple discharge. Bilateral multipore blood negative, expressed only nipple discharge is common and need not be assessed with ductogram and is best categorised as benign physiologic discharge.
Leis found 14.3% of patients with surgically significant discharge had biopsy proven cancer. Cancer was found in 33.3% clear/ watery discharge, 27.5% bloody/ sanguineous discharge, 12.9% pink/ serosanguineous discharge, 5.9% yellow/ serous discharge.
Solitary papillomas are the most common cause of spontaneous nipple discharge. These grow within a duct. Mammograms are usually normal. Rarely papilloma may have associated coarse calcification. On ductogram, these may commonly present as intraductal filling defects, complete ductal obstruction, ductal expansion with apparent distortion and irregularity of the wall. ‘Ducts containing papilloma frequently attenuate rapidly proximal to the lesion without significant branching/ distribution and are often dilated distally towards the nipple’ as in our case.
Ductogram findings of malignancy may be complete ductal obstruction, may associate with a mass at site of obstruction, filling defects, focal or diffuse ductal wall irregularity, periductal contrast extravasation and displacement of otherwise normal ducts [,radiology 1991 carda]. However, there is no specific imaging finding to separate papilloma and carcinoma.
To differentiate between papillomas and carcinoma are sometimes difficult even by core biopsy or fine needle cytology. Liberman et al found that surgery revealed cancer in 14% and high risk lesions in 17% in their series of patients who had benign concordant diagnosis of papilloma at percutaneous biopsy. Guenin described the use of vacuum assisted biopsy sampling for suspected solitary benign papilloma. However, the patient would need further surgical excision if the finding is discordant with the pathology result. Therefore, common current practice is surgical ductoscopy and microdochetomy/ duct excision without percutaneous biopsy.