Answer of May 2011
Clinical History:
A 58 year-old Chinese lady presented with vomiting, fluctuating mental status and on-and-off fever for 2 weeks. Physical examination did not reveal any neurological deficit. CT and MRI of the brain were performed.
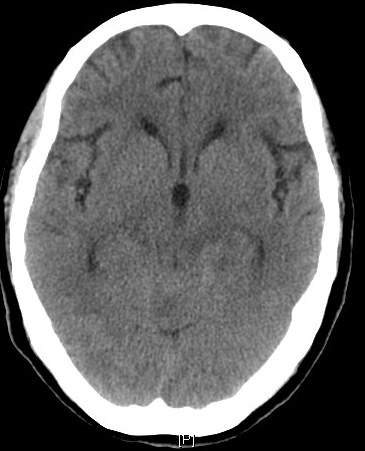
Axial plain CT brain Axial plain CT brain
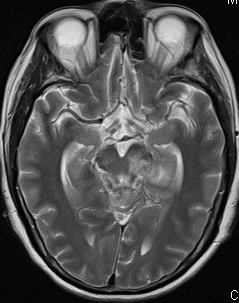
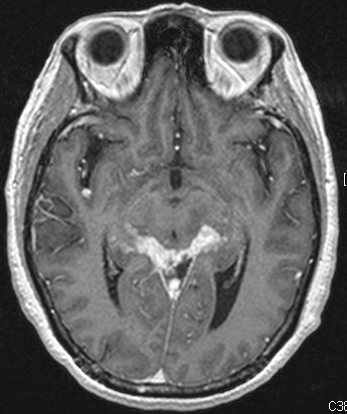
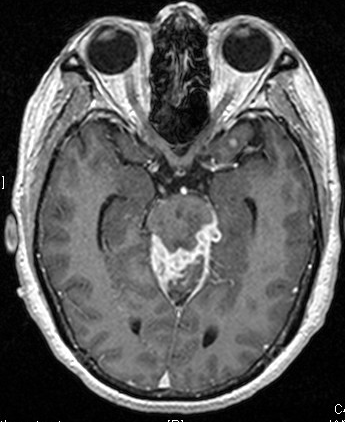
T2W axial MRI brain T1 post-Gadolinium axial MRI brain
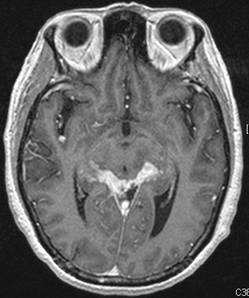
T1 post-Gadolinium axial MRI brain T1 post-Gadolinium axial MRI brain
Diagnosis:
Tuberculous meningitis
Discussion:
The diagnosis of our case is tuberculous meningitis. Although seen in all age groups, there is a peak incidence in children 0 to 4 years of age in high prevalence areas. In low prevalence areas it is more frequently encountered in adolescents and adults. Important risk factors include immunosuppression, HIV infection, diabetes mellitus and alcoholism.
Tuberculous infection of the central nervous system can have different types of manifestation, depending on the location of the tubercle. Those which rupture into the subarachnoid space cause meningitis. The gelatinous exudate infiltrates the cortical or meinigeal blood vessels, causing vasculitis and ischaemic infarction in approximately one-third of the cases. In this patient, left midbrain infarct is seen which is not evident in previous scans. Basal meningitis frequently results in cranial nerves deficits, most commonly affecting the 3rd, 4th and 6th cranial nerves. Obstructive hydrocephalus is common.
The diagnosis of tuberculous meningitis cannot be made or excluded on the basis of clinical findings. A high index of clinical suspicion is required for diagnosis. Acid-fast bacilli are seen in only approximately 25% of CSF smears.
Imaging plays an important role in aiding diagnosis of tuberculous meningitis. CT and MRI of the brain may show hydrocephalus, basilar meningeal thickening and enhancement, infarcts, edema and tuberculoma formation, which can appear as nodular enhancing lesion with a central hypodensity.
Treatment is by anti-tuberculous chemotherapy. The benefits of adjuvant corticosteroids remain in doubt. Treatment of complications e.g. drainage of hydrocephalus should also be done promptly.
Neurosarcoidosis can also give rise to nodular dural thickening and enhancement. Sarcoidosis most frequently affects blacks and less commonly Caucasians. It is rarely reported in China, south-east Asia or in the Middle East. CNS involvement occurs in 1-8% of patients with sarcoidosis and up to 15% in autopsies.
Abnormal meningeal enhancement can also be seen in cases of leukaemic infiltration as well as other kinds of leptomeningeal carcinomatosis, for example due to primary intra-cranial malignancies, metastases from carcinoma of the breast and bronchogenic carcinoma. A known history of primary tumour is often present. Carcinoma cells in the CSF are diagnostic, with the exception of a few false-positive results in patients who have reactive lymphocytes because of an infectious or inflammatory process in the CSF, and distinguishing between these lymphocytes from malignant lymphomatous cells is difficult.
Meningioma is an extra-axial brain tumour which has an obtuse angle with the adjacent dural surface. The commonest type is globular meningioma, commonly presented as a well-defined slightly hyperdense mass with intense contrast enhancement. Internal calcification and local mass effect may be present. Atypical presentation of meningioma includes meningioma en plaque, which often produces pronounced hyperostosis of adjacent bone particularly along the skull base.