Answer of August 2012
Clinical History:
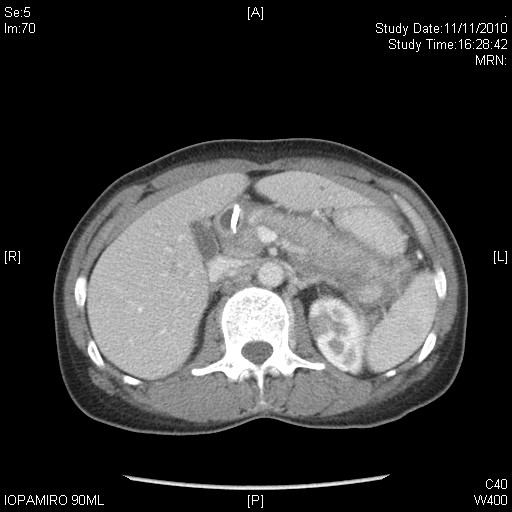
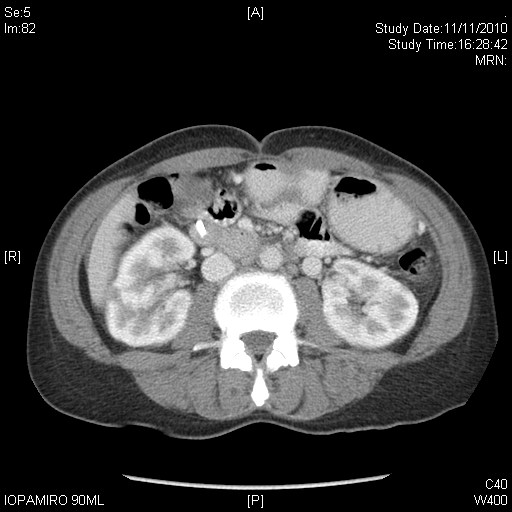
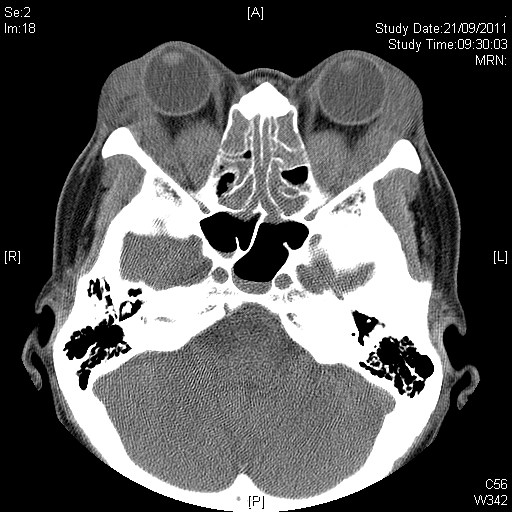
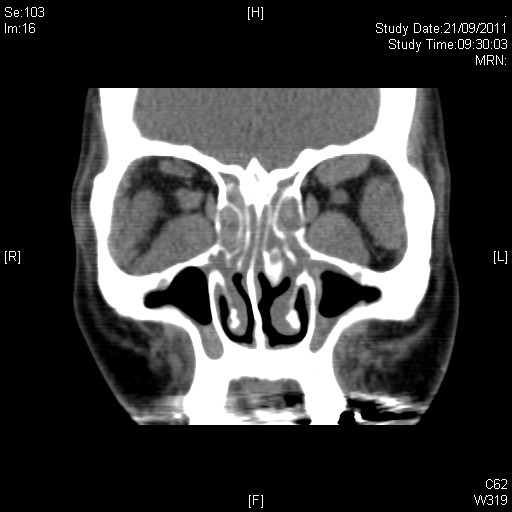
This 53-year-old lady, with unremarkable past health, presented with bouts of epigastric pain and tea-coloured urine. Endoscopic retrograde cholangiopancreatography (ERCP) revealed dilated intrahepatic ducts and a stricture in the lower common bile duct (CBD) which prompted stent placement (blue arrow in the first image) and a brush cytology which came back negative. Abdominal CT performed at presentation and 6 months later showed essentially static features (images from the later set of CT is shown). Meanwhile, this lady was also seen by ophthalmologists for painless proptosis of a few years' duration.
Diagnosis:
IgG4 positive systemic autoimmune disease with pancreatic, biliary, renal and orbital involvement.
Discussion:
Autoimmune pancreatitis (IgG4-positive systemic autoimmune pancreatitis) is a distinct type of chronic pancreatitis, characterised by abundant IgG4+ plasma cells leading to fibrosis. Occurrence is uncommon, accounting for 11% or less of chronic pancreatitis cases. Mean age of presentation is 60 years, with a twofold predilection for men. Typical presenting features include fluctuating obstructive jaundice, vague epigastric pain, weight loss, steatorrhoea, and diabetes. IgG4 levels are elevated in ~80%. Extrapancreatic manifestations are common. Rapid improvement of clinical and imaging abnormalities typically follows 3-4 weeks of steroid therapy.
Diagnostic Criteria, devised by Kim et al in 2006, include:
• Characteristic imaging features . enlargement of pancreas, irregular segmental narrowing of MPD.
• Raised serum IgG4 levels or presence of autoantibodies.
• Characteristic histopathological findings
• Response to corticosteroids.
(For diagnosis: radiological criterion + at least one of the other three criteria are required.)
On imaging, two main types predominate . the focal type and the diffuse type. The focal type is slightly more common (accounting for 49%), and most often presents as a solitary mass in the proximal pancreas. Differentiation from carcinoma is unreliable by imaging, and biopsy is necessary for diagnosis in such instances.
The diffuse type (accounting for 44%) shows diffuse pancreatic swelling mimicking acute pancreatitis, but there is a distinctive lack of peripancreatic stranding and fat necrosis, and presence of a peripancreatic halo.
Biliary involvement is the most common form of extrapancreatic manifestation (77%), and most often affects the intrapancreatic portion of the CBD. Renal lesions (35%) are most often cortical nodular or wedge-shaped lesions resembling cysts, and can be difficult to distinguish from lymphoma. Mass-like lesions and diffuse thickening of the urothelium are also possible appearances.
Craniocervical manifestations are highest in incidence in the salivary glands (14%), manifesting as Mikulicz.s disease. Thyroid involvement (12%) may manifest as either Riedel.s or Hashimoto.s thyroiditis. Orbital involvement is uncommon (3%) and predominates in the lachrymal glands.
Of the choices of possible answers provided, IgG4-positive pancreatitis is the most plausible diagnosis accounting for diffuse pancreatic swelling, peripancreatic halo, and biliary stricturing. Intra-abdominally, amyloidosis most commonly affects the intestine, especially the colon, and sarcoidosis most often manifests in the stomach and lymph nodes; Pancreatic involvement is uncommon in either of these entities. Lymphoma can produce identical renal lesions lacks a tendency to involve the pancreas, and is usually accompanied by prominent lymphadenopathy.