Answer of May 2012
Clinical History:
An 46 years old lady presented with progressive bradykinesia, rigidity, and gait difficulty for 2 years. Patient did not response to treatment, and subsequently demonstrates symptoms progression with new onset of orthostatic hypotension and urinary retention.
MRI brain was performed to rule-out organic cause.
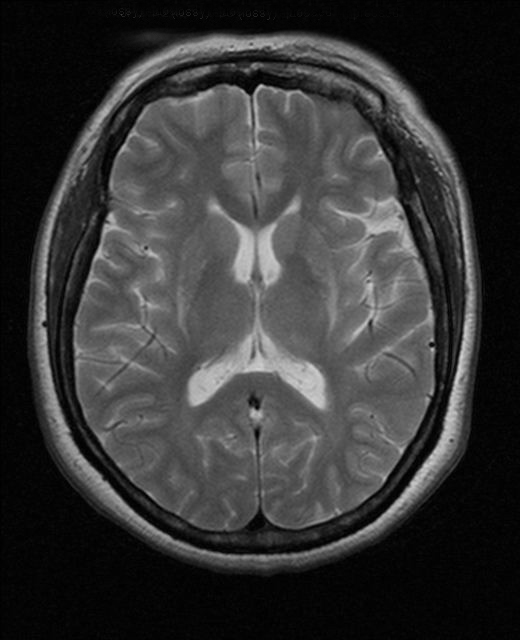
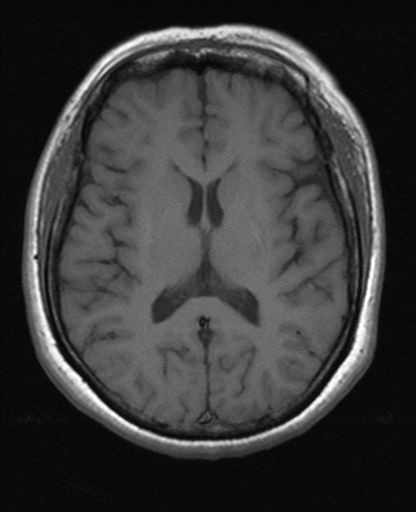
T2-weighted axial images
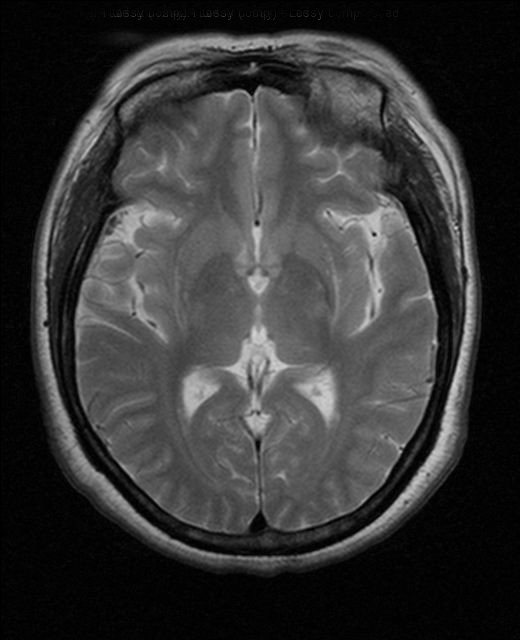
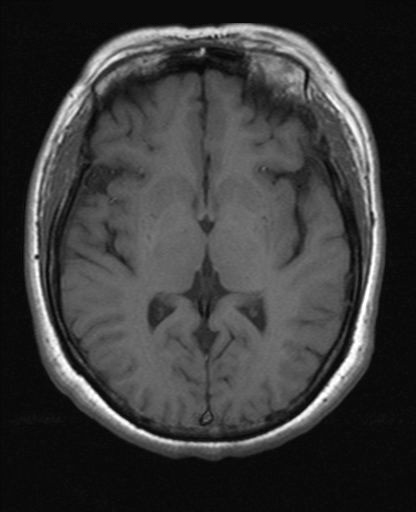
T2-weighted axial FLAIR images
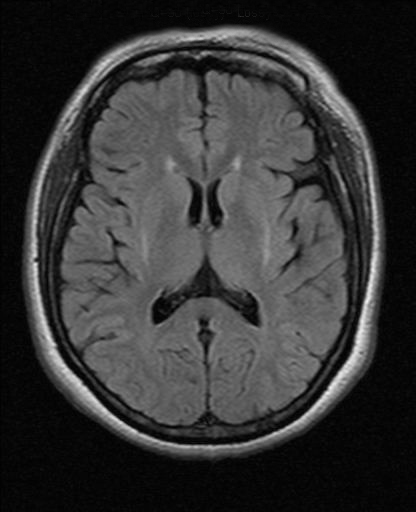
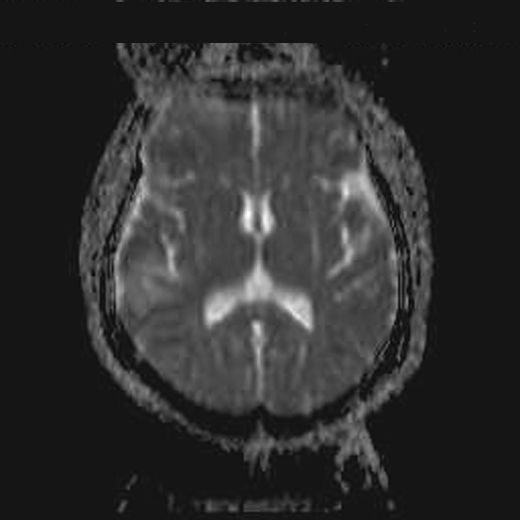
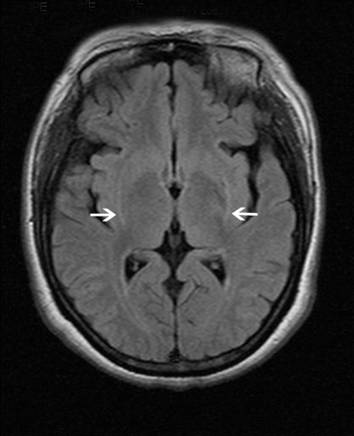
T1-weighted axial image.
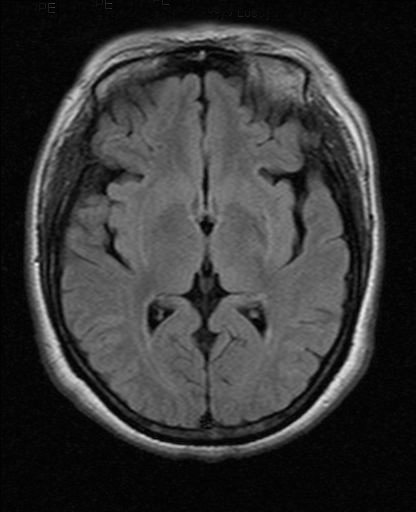
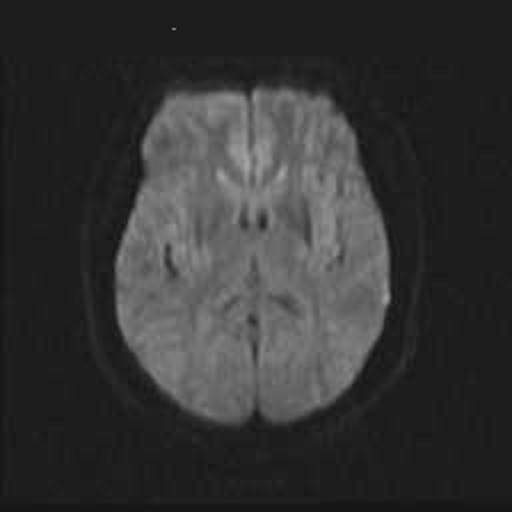
Diffusion weighted image and ADC map
Diagnosis:
Multiple system atrophy - Parkinson variant (Striatonigral Degeneration)
Discussion:
Multiple system atrophy (MSA) is a sporadic, progressive, adult-onset disorder associated with various degrees of dysfunction of the extrapyramidal, cerebellar, and autonomic systems. MSA can be further classified according to clinical presentation into MSA-Parkinsonism (Striatonigral Degeneration), MSA-Cerebellar type (Olivopontocerebellar Degeneration) and MSA-Autonomic failure (Shy Drager Syndrome). In neuropathologic examinations, the Parkinson variant of MSA(MSA-P) is characterized by selective neuronal loss and gliosis predominantly affecting the basal ganglia, substantia nigra, olivopontocerebellar pathways, and intermediolateral cell columns of the spinal cord. The clinical differentiation of MSA-P from Parkinson disease (PD) and other atypical parkinsonian disorders, such as progressive supranuclear palsy (PSP), is challenging and imaging plays an important role. Early differentiation of these diseases is important, however, to establish differences in their natural history and treatment response. In clinical practice with patients diagnosed with MSA-P, clinicians should consider symptoms in addition to parkinsonism (eg, orthostatic hypotension, urinary retention, and respiratory disturbances). There is increasing evidence that MR imaging is useful to establish an accurate diagnosis. The abnormal putaminal findings that characteristically differentiate patients with MSA from those with other parkinsonian disorders and control subjects are well known: a hyperintense putaminal rim on T2-weighted images, putaminal hypointensity on T2-weighted images, and putaminal atrophy. In some patients, however, an unequivocal diagnosis cannot be made with MR imaging findings alone. Putaminal hyperintensity on T1-weighted images is frequently observed in patients with MSA-P.
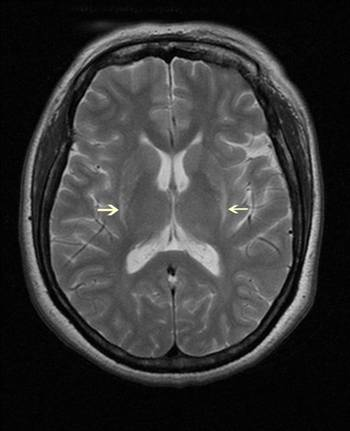
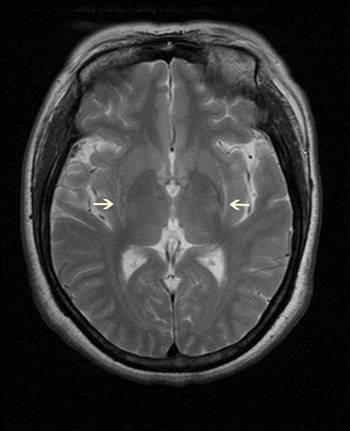
T2-weighted axial images of this patient showed putaminal atrophy, noticed by linearization of posterolateral margin of the putamen and decreased width of the putamen. Abnormal hyperintense signals are seen along the posterolateral margin of bilateral putamen.
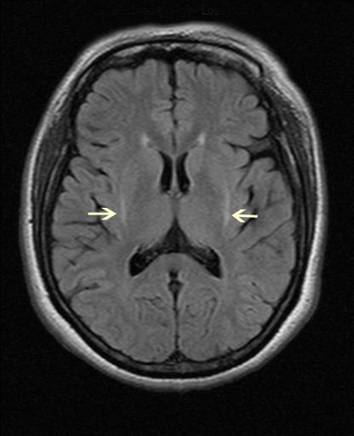
T2-weighted axial FLAIR images showed similar findings with abnormal hyperintense signals along the lateral margin of the putamen.
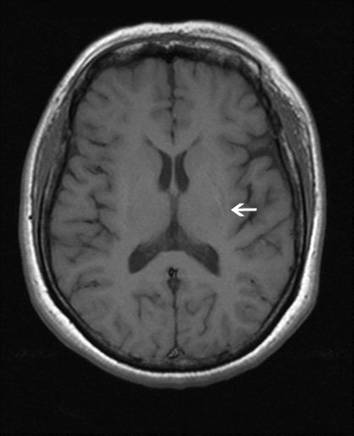

T1-weighted axial image of the same patient showed subtle high-intensity signals at posterolateral margin of bilateral putamen.
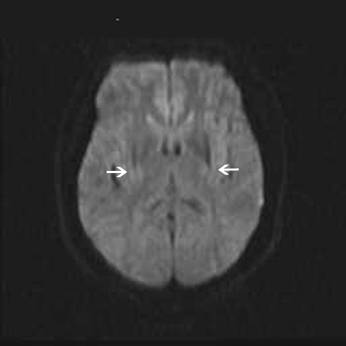
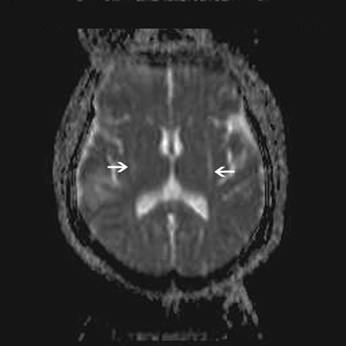
Diffusion weighted images showed increase diffusivity around bilateral putamen.