Answer of August 2013
Clinical History:
A 51-year-old lady presented with left neck swelling. Physical examination showed a soft and non-tender left upper neck mass. Flexible laryngoscopy found a smooth left parapharyngeal mass, partially obstructing the airway. CT and MRI of the neck were performed.
Diagnosis:
Schwannoma
Discussion:
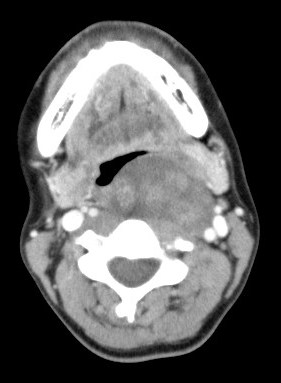
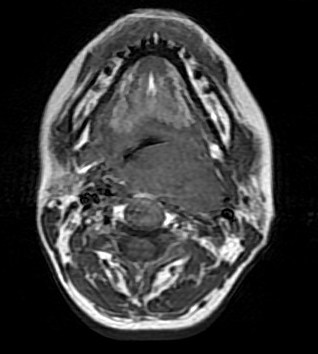
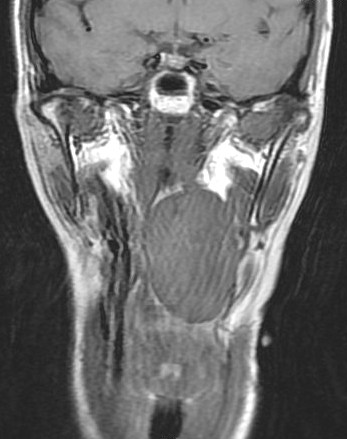
Contrast enhanced CT and MRI of the neck showed a well circumscribed heterogeneously enhancing lesion at the left parapharyngeal space displacing the left carotid artery and jugular vein laterally. Excision of the tumor was performed. Pathological examination confirmed diagnosis of schwannoma.
Primary tumors of the parapharyngeal space are rare, the most common type is neurogenic tumor. Schwannoma is the most common type of parapharyngeal neurogenic tumors, accounting for 55% of them. Most of the parapharyngeal schwannomas are benign and the majority of them arise from the vagus nerve and cervical sympathetic chain. Parapharyngeal space schwannomas usually occur between the ages of 30 to 60 years. A 3:1 male-female ratio has been reported for cervical sympathetic chain schwannomas and no gender predisposition for vagal nerve schwannomas has been reported. Most patients present with a slowly enlarging firm, painless mass in the lateral neck, similar to this case. Some patients also present with pressure symptoms, hoarseness and cough.
Preoperative imaging diagnosis of parapharyngeal schwannoma is often difficult. On CT, it appears as a well-defined mass, usually of lower attenuation than muscle, as demonstrated in this case. Contrast enhancement may be homogenous or heterogeneous. On MRI, it is a well-defined lesion showing low signal on T1-weighted images and high signal intensity on T2-weighted images which is seen in this case. Evidence of necrosis and cystic degeneration could sometimes be seen. Schwannomas from the poststyloid parapharyngeal space tend to displace the carotid sheath structures anteromedially. Whereas, schwannomas from the prestyloid parapharyngeal space tend to displace the carotid sheath structures posterolaterally.
Due to their slow growth and noninvasive nature, an observational approach may be considered for parapharyngeal schwannomas. In cases where the tumors exert pressure effect on the adjacent tissues, complete surgical resection is the treatment of choice.
This case is unlikely to be a carotid body tumor as this tumor does not arise from the carotid bifurcation and does not splay the external and internal carotid arteries. Also, this case does not demonstrate intense enhancement on CT and MRI which is typical for carotid body tumor. In addition, this case does not show the ‘salt-and-pepper’ appearance (flow voids) in MRI which is classical for a carotid body tumor.
This case is unlikely to be a brachial cleft cyst as it is not of significant cystic density/signal which would be expected in a brachial cleft cyst. Also, this lesion shows heterogeneous enhancement which is not typical for brachial cleft cyst.
The preserved fat plane between the lesion and the deep lobe of the parotid gland indicates that the mass is extraparotid. Therefore, it is unlikely to be a parotid gland tumor.
This case is not likely a cystic hygroma as it is not of significant cystic density/signal which would be seen in a cystic hygroma. Also, cystic hygroma is a soft lesion showing no significant displacement of surrounding structures and it has an irregular shape. These features of cystic hygroma are not seen in this case.