Answer of May 2013
Clinical History:
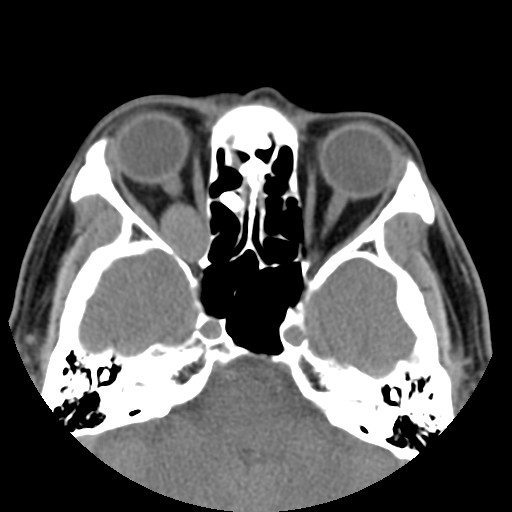
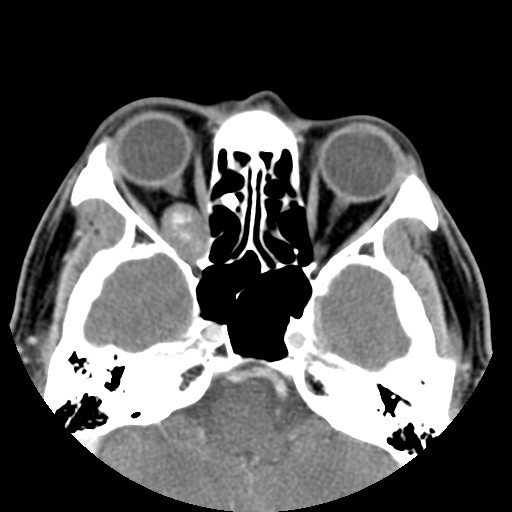
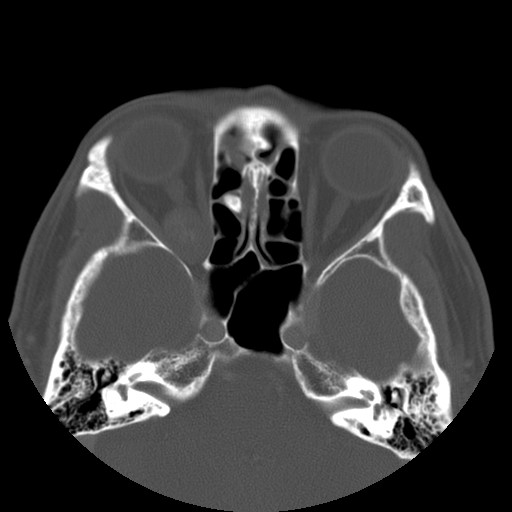
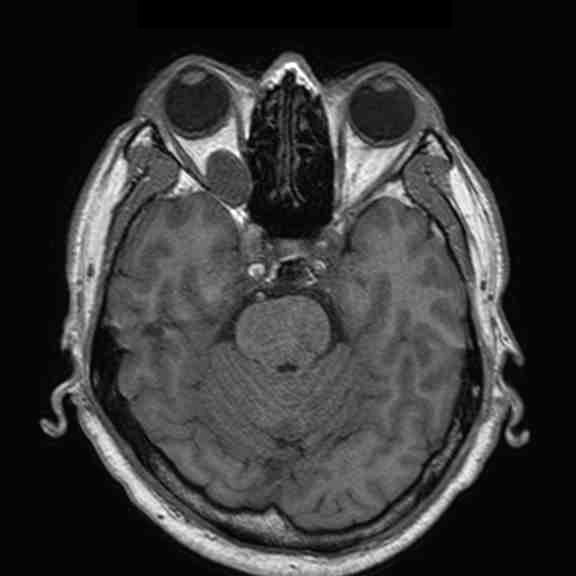
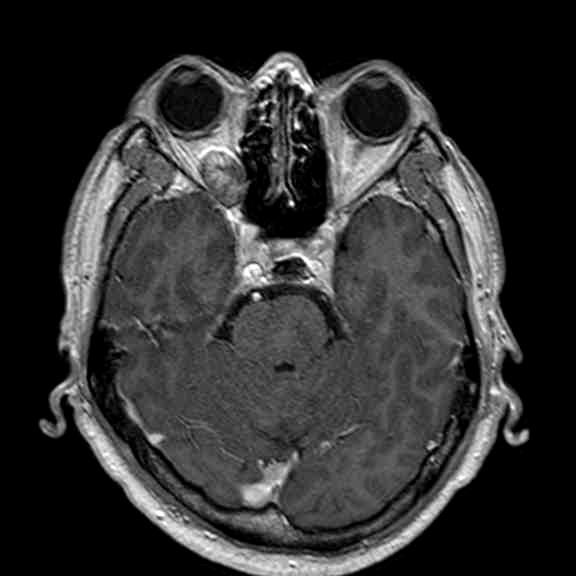
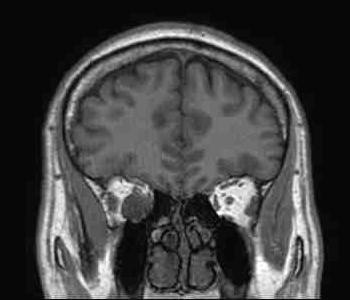
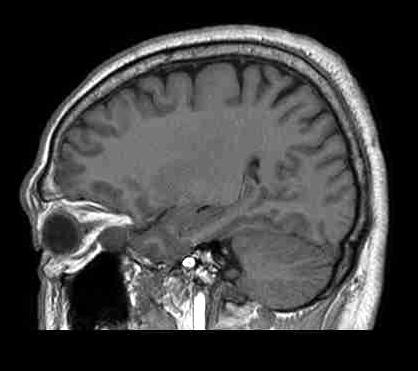
A 58-year-old gentleman presented with recent deterioration of right eye visual acuity and proptosis.
CT and MRI were performed.
Diagnosis:
Orbital cavernous haemangioma
Discussion:
Orbital cavernous haemangioma is the most common adult orbital mass lesion, in this case presenting in an unusual location but with typical imaging features.
It is a low-flow venous malformation of the orbit characterized by endothelial-lined cavernous spaces, and is distinct from capillary haemangioma, a neoplastic tumour of infancy which involutes with age. It has a female predominance, age ranging from 18-72 years (mean age 43-48 years). Associations with Maffucci syndrome and blue rubber bleb naevus syndrome have been reported. Classically, the patient presents with progressive painless proptosis, and may have diplopia, visual impairment or increased intra-ocular pressure. It is mostly intra-conal in location (80%), usually in the lateral retro-bulbar intra-conal space, but can occur anywhere in the orbit, including extra-conal, intra-mucuslar, or even intra-osseous arising within the orbital bone. It is usually round or ovoid, lobulated, with sharp demarcation. It has a fibrous pseudocapsule.
CT: It is usually homogeneously isodense, and may be hyperdense due to microcalcifications. However, coarse punctuate macrocalcifications or phleboliths are not typical. Adjacent structures are displaced but not invaded. There is often benign bone remodeling in larger lesions, owing to its slow growth. It usually demonstrates patchy avid enhancement, as in this case.
MR: On T1WI, it is homogeneous and isointense to muscle, and may have a hypointense rim which represents the pseudocapsule. On T2WI, it is hyperintense and may show internal septations. Post-Gadolinium, it exhibits heterogeneous early patchy central enhancement, and may show delayed fill-in. However, it is usually not visible on routine MRA since it is a low-flow lesion.
Angiogram: It is essentially isolated from the systemic circulation and does not show distinct tumour blush. There may be delayed contrast pooling.
Differential consideration depends on the location (e.g. intra- vs extra-conal) and imaging features, but would generally include optic nerve sheath meningioma, optic nerve glioma, schwannoma, haemangiopericytoma, lymphoma & metastasis, orbital varix, lymphangioma, pseudotumour, lacrimal gland tumours, haematoma, sarcoidosis etc.
Symptomatic cases of cavernous haemangioma (visual disturbance, cosmesis, significant mass effect) are treated by surgical resection. The pseudocapsule facilitates complete resection with excellent prognosis and low recurrence rate.