Answer of April 2013
Clinical History:
A 56 female patient who enjoys good past health presented to the ophthalmology specialist clinic for blurring of right eye vision for 2 months. Right fundal examination reveals an intraglobular lesion demonstrating some pigment or discoloration. CT scan of the orbit was performed.
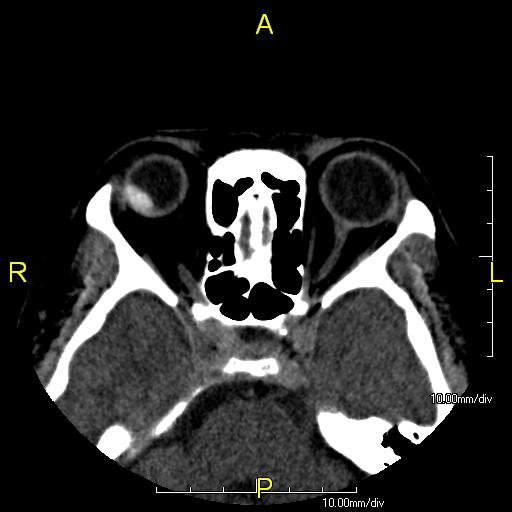
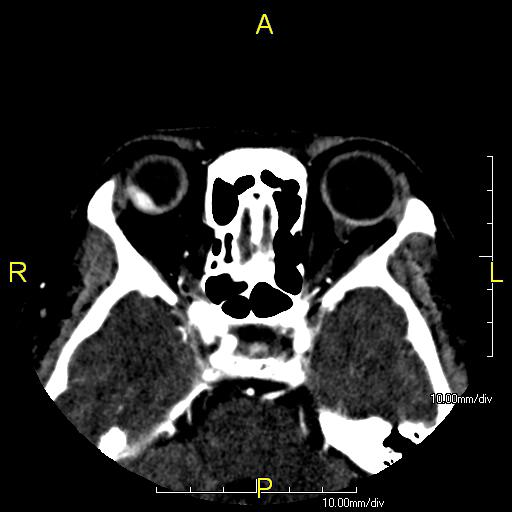
Axial non-contrast
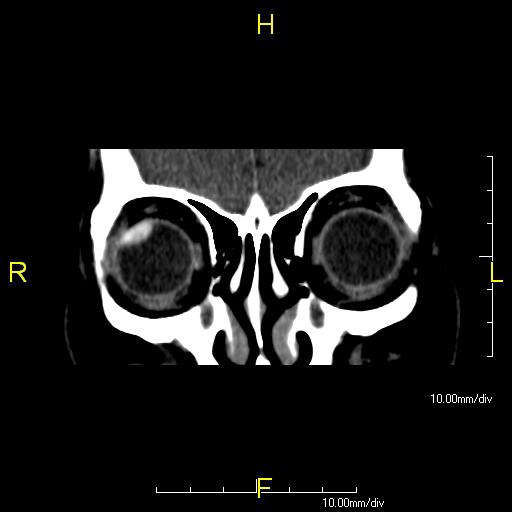
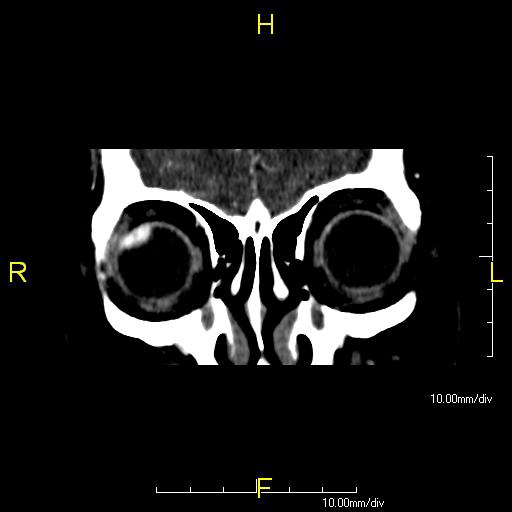
Coronal non-contrast
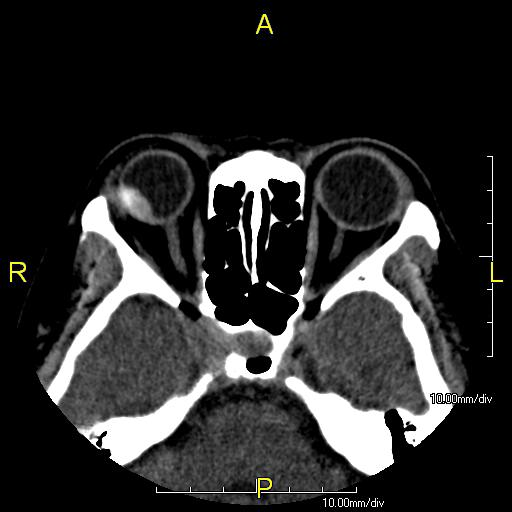
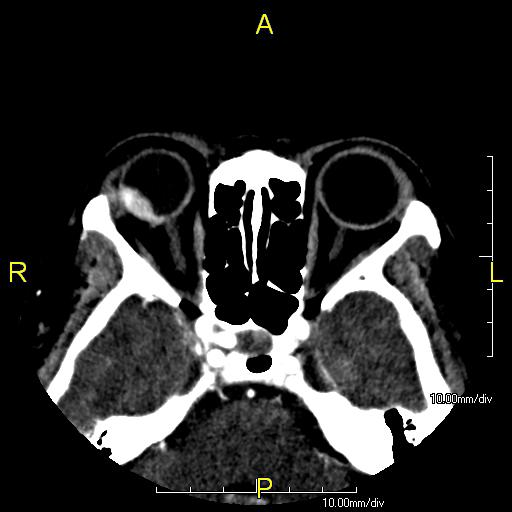
Axial post-contrast
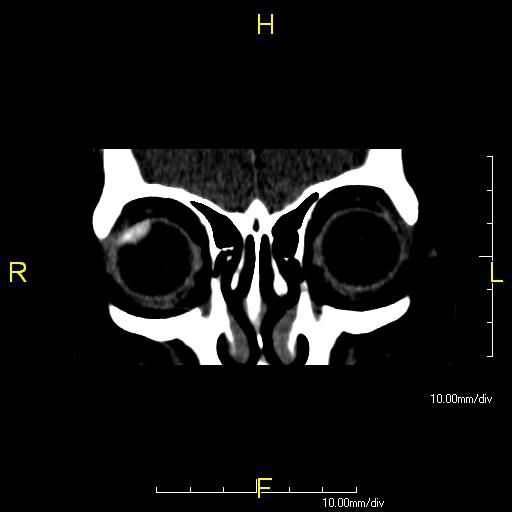
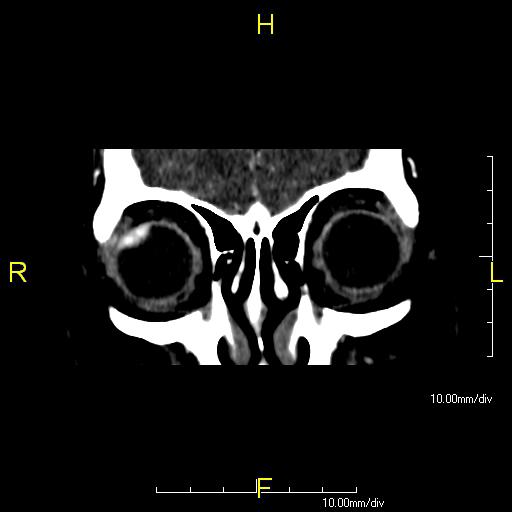
Coronal post-contrast
Diagnosis:
Choroidal melanoma
Discussion:
Uveal melanoma is the most common intraocular tumor is adults. Melanomas may occur in any of the three subdivisions of the uvea: the iris, the ciliary body and the choroid. The choroidal subtype is most common, accounts for about 85% of uveal melanomas. Melanomas involving the ciliary body and choroid are thought to arise from preexisting melanocytic nevi. These tumors are most common among people of northern European descent while they are rare in African descent and are uncommon in Asian and Hispanic descents.
The most common presentation of uveal melanoma is painless vision disturbance although some patients may be asymptomatic. This entity has a slight male preference and the peak incidence is in the 6th decade. Factors that are indicative of unfavorable prognosis include increasing tumor size, extraocular growth, infiltration of the ciliary body and intense pigmentation.
At unenhanced CT, the lesions appear elevated, hyperattenuating and sharply marginated. They show diffuse moderate enhancement after contrast administration. Calcifications are rare but may appear after therapy. In MR imaging, most choroidal melanomas appear as well-defined solid masses. Because of the paramagnetic effects of melanin, intensely melanotic melanomas have shorter T1 and T2 relaxation times, producing increased signal intensity on T1-weighted images and markedly decreased signal intensity on T2-weighted images.
Small non-progressive melanomas (<3mm thick) can be followed every 3-6 months with ultrasound examination. Small and medium progressive tumors (3-10mm thick) can be treated with plague brachytherapy or external beam radiation therapy with charged particles. Surgical enucleation is warranted for all large melanomas (>10mm ). The patient in this case has undergone surgical enucleation.
The main differential in this case is choroidal metastases (from lung, breast, hypervascular and hematologic malignancies), which are frequently bilateral (33%) and multiple. Choroidal metastases are usually depicted as broad-based flat lesions. At MR imaging, they tend to be iso- to hyperintense on T1WI and hyperintense on T2WI. And obtaining a clinical history is mandatory for any known history of primary malignancy.
Another main differential is choroidal hemangioma. At CT, circumscribed choroidal hemangiomas in the absence of retinal detachment appear as ill-defined masses that exhibit intense enhancement after the administration of contrast material. At MR imaging, most of them are hyperintense to that of vitreous in T1WI and in T2WI FSE, they are typically hyperintense, usually appearing isointense to that of vitreous.
Chrorioretinal detachment doesn't enhance while retinoblastoma only occurs rarely in adults and is commonly associated with calcifications (95%). These make them the wrong options.