Answer of February 2013
Clinical History:
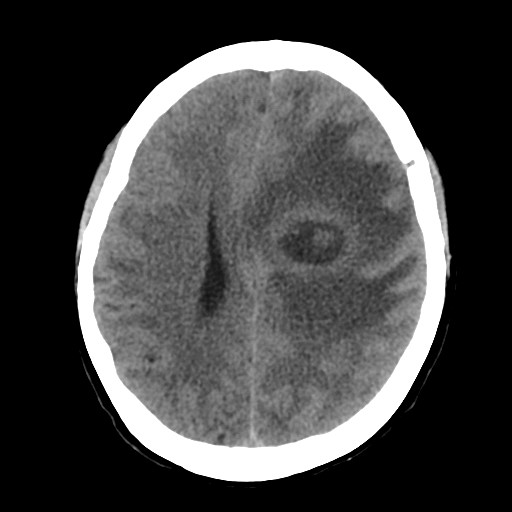
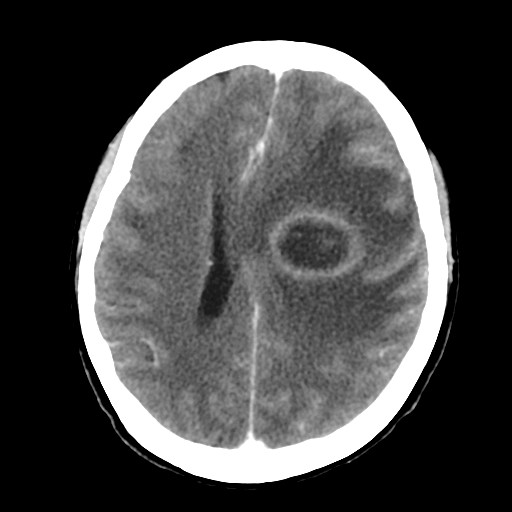
A 70-year-old lady present with right sided weakness and fever. CT brain with contrast was performed.
Plain Contrast
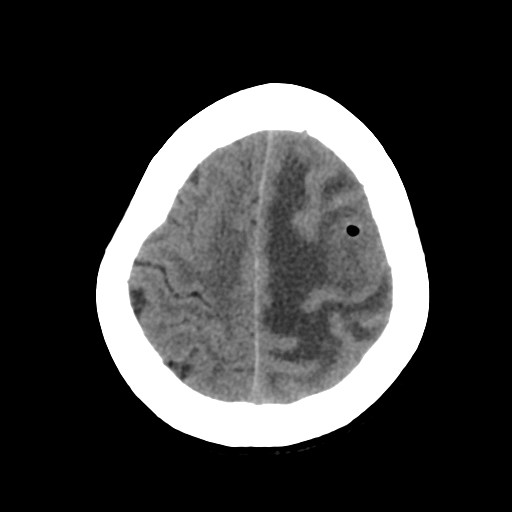
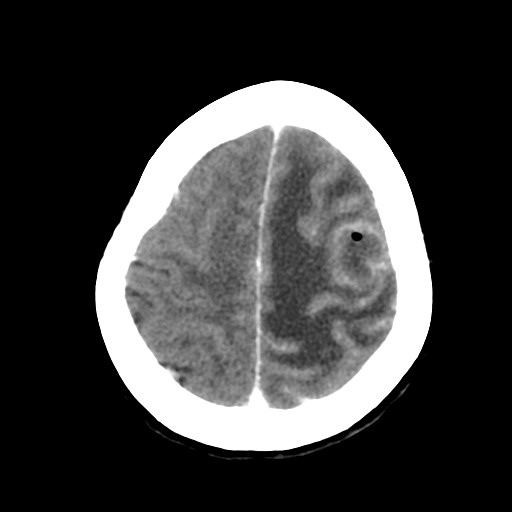
This is the patient.s chest X ray. CT thorax with contrast was performed as an abnormality is noted on CXR.
MIP images from CT thorax with contrast
Diagnosis:
Pulmonary arteriovenous fistula complicated with brain abscess
Discussion:
Pulmonary arteriovenous fistula (PAVF) is an abnormal vascular communication between pulmonary artery and vein (95%) or systemic artery and pulmonary vein (5%). They are usually congenital with defect of capillary structure. They could be acquired in patients with cirrhosis, trauma, post-surgery. Commonly they occur over lower lobes. They usually occur as isolated abnormality. Multiple lesions are known to be associated with Osler-Weber-Rendu syndrome or Hereditary haemorrhagic telangiectasis. On plain radiographs, PAVF occur as round, or lobulated lesion of uniform density with connecting tubular structure / vessels to hilar vessels. Calcification is rare. On CT, homogeneously enhanced feeding artery and draining vein with connection to pulmonary artery and pulmonary vein are usually seen. Angiography is performed when embolization is contemplated.
Patients with PAVF are usually asymptomatic till adulthood (3rd or 4th decade). CNS symptoms are commonly the initial manifestation, like cerebrovascular accident (ischemic stroke, TIA) and brain abscess, due to absence of filter effect of capillaries in pulmonary circulation on emboli or septic emoboli. Sometimes patient may have chest symptoms, like hemoptysis, shortness of breath, especially if there are multiple PAVF or if they are large, which produces right to left shunt and hypoxia.