Answer of April 2015
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinial History:
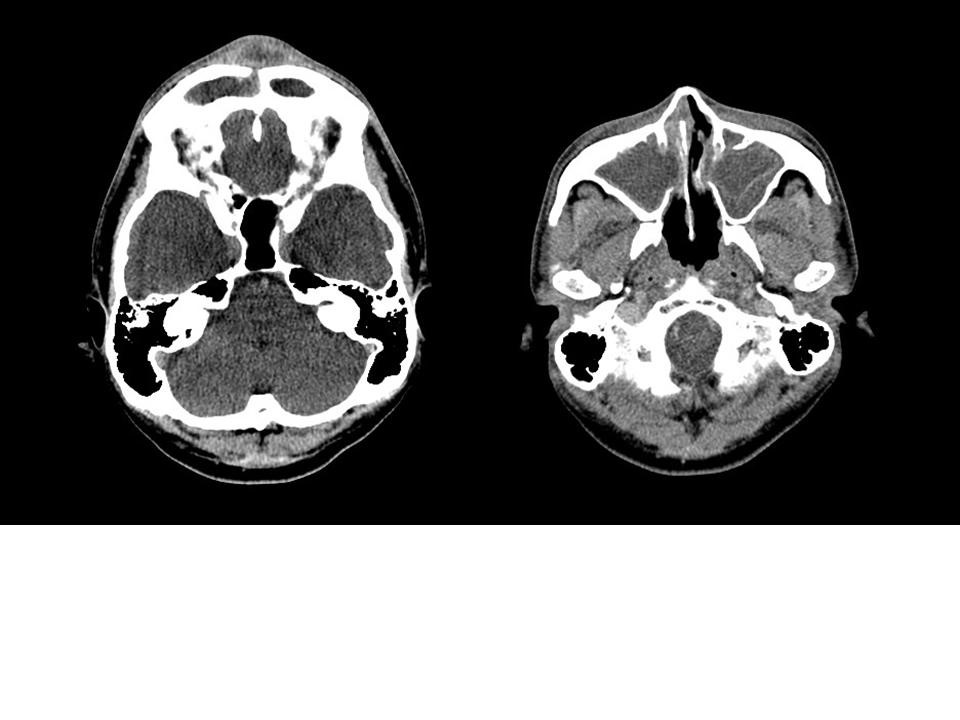
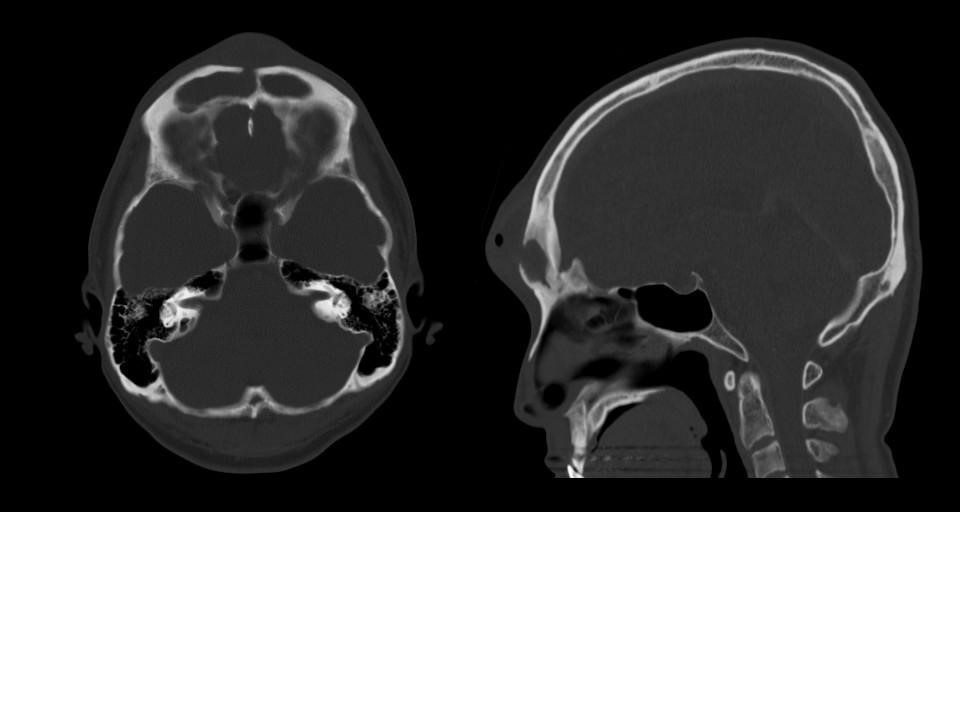
A 34-year-old with good past health presented with 2 months history of nasal discharge and progressive fronal swelling for 10 days. (4 images: contrast CT axial soft tissue windows X 2, axial bone window X 1, sagittal X 1)
Diagnosis:
Discussion:
Frontal sinusitis can involve frontal bone either by direct extension or by thrombophlebitis of the diploic veins. Involvement of bone marrow can result in osteomyelitis, which subsequently result in PPT. [1] Both acute and chronic frontal sinusitis can cause PPT. Microbiological examination often yielded multiple growth, including anaerobes [2], but the most common organisms were streptococci and staphylococci. Sterile cultures were also common as most patient received antibiotics treatment before surgery. [3]
Clinical presentations includes headache, forehead mass and rhinorrhea and systemic symptoms such as fever.
The most common complications of PPT are intracranial complications, which include epidural abscess, subdural empyema, meningitis, brain abscess and dural sinus thrombosis. [4, 5] Orbital complications are not uncommon in PPT patients. The most common orbital complication is periorbital/preseptal cellulitis. Others include orbital cellulits, orbital subperiosteal abscess and orbital abscess. [3]
Prompt diagnosis and treatment is vital in view of high rate of complications. Imaging like CT and MRI aids in the diagnosis of PPT and its complications. Successful treatment includes timely surgical interventions with drainage of abscesses and affected sinuses and debridement of infected bone. High dose intravenous antibiotics with both aerobic and anaerobic coverage should also be commenced. Subsequent antibiotic regimen should be modified according to the culture results. A prolonged course of antibiotics at least 6-8 weeks is recommended.