Answer of March 2015
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 63 years old lady with history of osteoporosis complained about mild, painless swelling over her right lower shin for a few months. She had no history of trauma, no fever or weight loss. Physical examination was unremarkable. Plain radiograph of her right leg was performed as initial workup, (Picture 1 and picture 2), followed by NM/CT study (Picture 3 and 4) and MRI study (Picture 5 and 6).
Picture 1
Picture 2
Picture 3
Picture 4
Picture 5
Picture 6
Diagnosis:
Parosteal Osteosarcoma
Discussion:
In plain film, at the distal fibular there is a lobulated and 'cauliflower-like' mass with dense ossification adjacent to bone. There is cortical thickening noted at the adjacent bone cortex. No definite cortical destruction is noted in plain film.
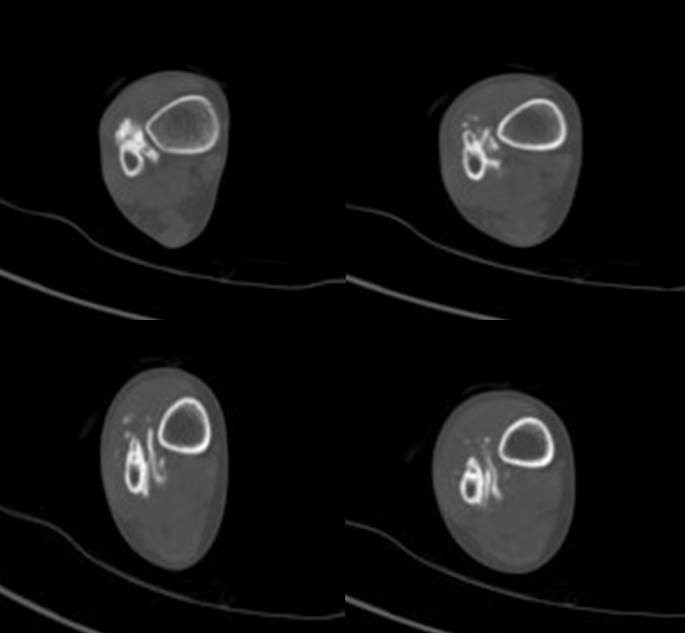
In CT, a stalk is clearly demonstrated connecting the bony cortex and this ossified mass.
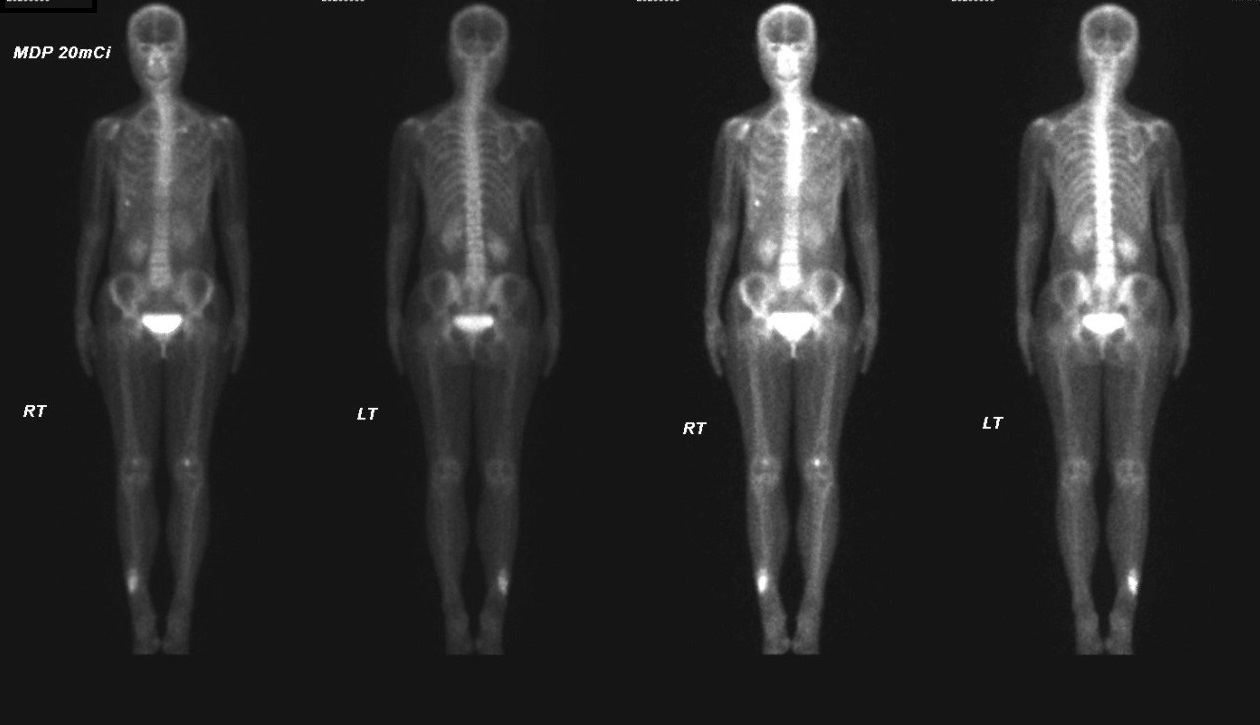
In bone scan, intense tracer uptake is noted in the right lower shin region, suggestive of increased osteoblastic activity. The uptake at right lower rib is likely due to rib trauma and the uptake in both knees is likely due to degeneration.
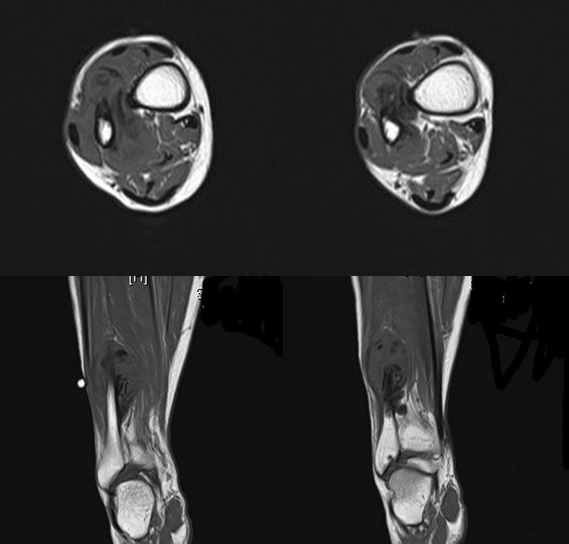
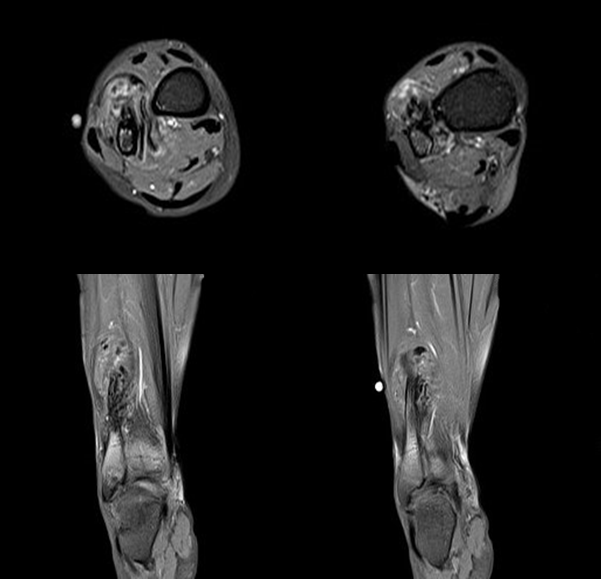
In MRI, a soft tissue mass with foci of enhancement is noted wrapping around the distal fibular. The ossification associated with this soft tissue mass appeared as low signal. The stalk connecting the boney cortex and the ossified mass is again noted. No definite abnormal marrow signal is noted in the adjacent bone.
Parosteal osteosarcoma is the most common type of juxtacortical osteosarcoma. It typically manifests in the 2nd to 4th decades of life. The tumor usually occurs in the metaphyses of long bones and the posterior aspect of the distal femur is the most frequent site.
Parosteal osteosarcoma originates from the outer fibrous layer of periosteum. It exhibits extensive bone matrix and minimal fibroblastic cellular atypia and is considered to be a low grade tumor.
Differential diagnostic considerations for parosteal osteosarcoma include benign entities such as osteochondroma and myositis ossifican. In contrast to osteochondroma, parosteal osteosarcoma lacks corticomedullary continuity between the tumor and the underlying medullary bone.
The ossification pattern of parosteal osteosarcoma is the inverse of that seen in myositis ossificans, with the densest ossification in the center of the lesion and the least radiopaque bone at the periphery
Parosteal osteosarcomas are usually low-grade lesions. It is usually treated with surgical resection and no neoadjuvant chemotherapy or radiation. As they are frequently metaphyseal in location, large parosteal osteosarcomas or those with deep medullary invasion may require limb salvage, including joint replacement.