Answer of June 2014
Clinical History:
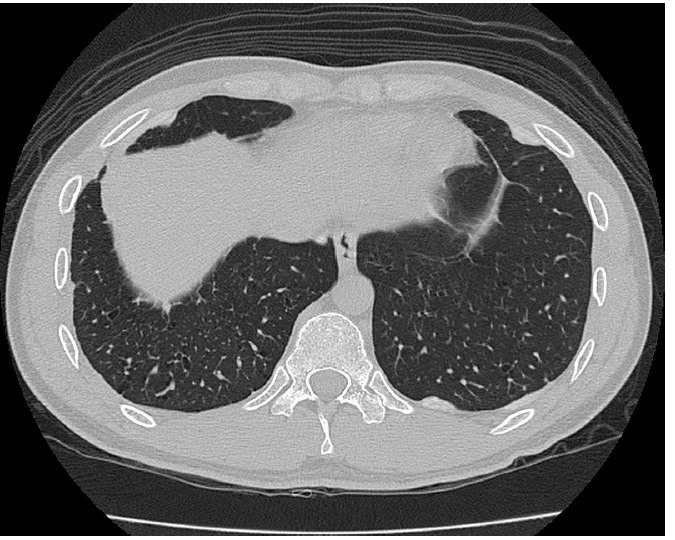
A 25 years old gentleman with unremarkable past health presented with acute onset of shortness of breath with chest pain. Chest X-ray on admission and subsequent high-resolution CT thorax taken a few months latter were available.
Diagnosis:
Pulmonary Langerhans cell histiocytosis (LCH) with bilateral pneumothoraces.
Discussion:
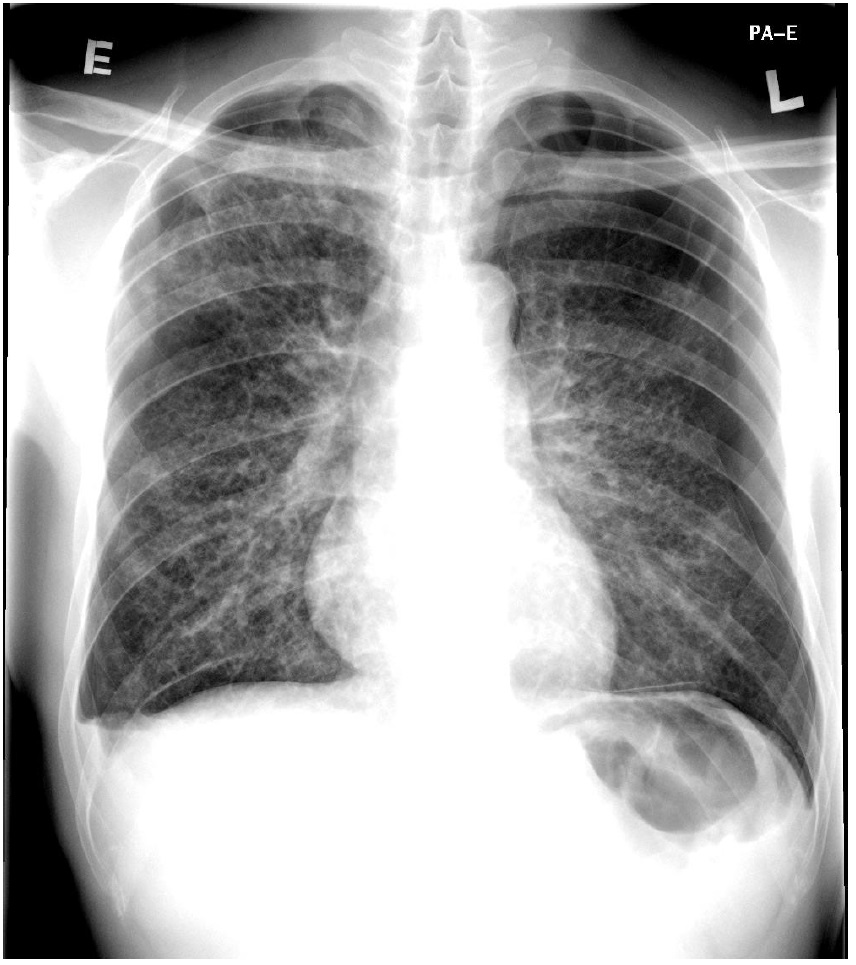
Chest
x-ray on admission revealed bilateral pneumothoraces with a background of diffuse
cystic lung changes in bilateral lung fields. Patient latter undergone VATS pleurodesis with resection of lung bulla
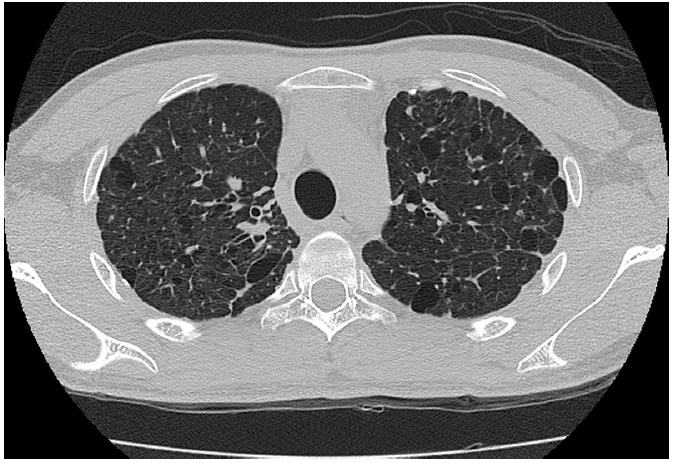
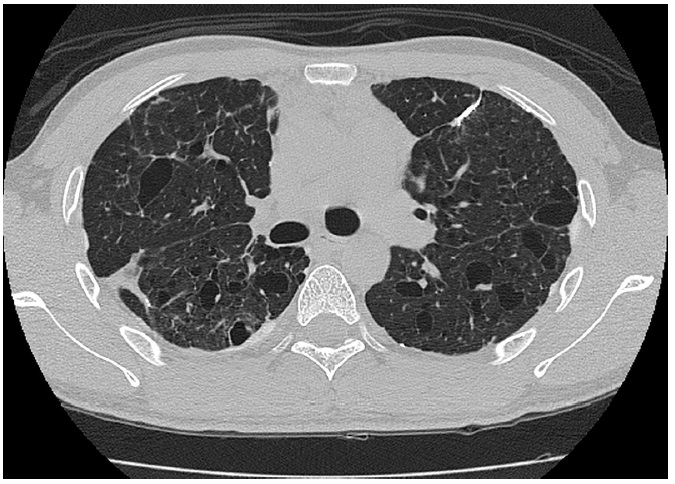
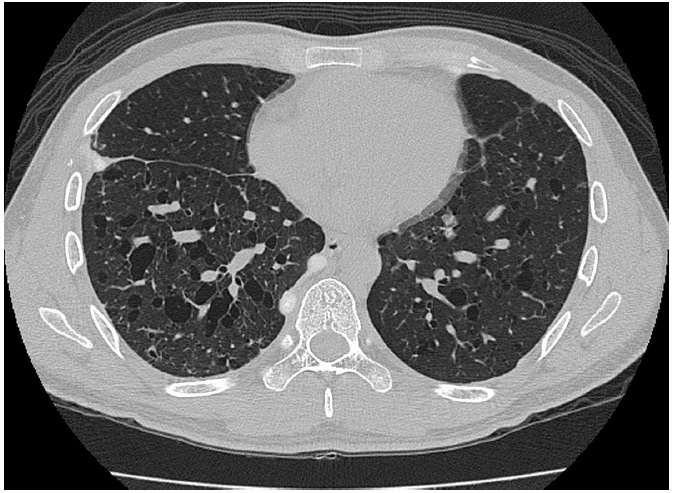
which histology confirmed the diagnosis of pulmonary LCH. Subsequent high-resolution CT thorax showed
presence of multiple thin-wall, irregular-shaped cysts in both lungs with upper
zone predominance and spare the lung bases. Small subcentimeter lung nodules were also seen bilaterally. Lung volumes were preserved.
Isolated
pulmonary LCH occurs predominantly in young adults, with a peak frequency
between 20 and 40 years ago. In the
contrary, multifocal and systemic forms of LCH are usually seen in infants and
children, and pulmonary involvement is not a prominent feature in these
patients. A male predominance of the
disease has been reported. Smoking is
highly related to the development of pulmonary LCH but no direct correlation
between the degree of cigarette consumption and disease severity has been
demonstrated.
Clinical
presentations of pulmonary LCH include dry cough and dyspnea on exertion. Acute presentation of chest pain is more
frequently a symptom of pneumothorax which can be seen in 10-20% of patients. Extrapulmonary manifestations of the disease can
include symptoms related to pituitary (e.g. diabetes insipidus), bone or skin
involvement. Not uncommonly, the disease
presents as an incidental finding on a routine chest x-ray and it has been
reported to represent up to 36% of patients. Physical examination is usually unremarkable
except for patients complicated with pneumothorax or cor pulmonale, or
presented with other extrapulmonary involvement.
Radiographic
features of pulmonary LCH vary depending on the stage of the disease. A
proposed progression of imaging abnormalities starts with solid nodules which
then become cavitary nodules, thick-walled cysts, thin-walled cysts and
confluent cysts. On initial stage,
multiple bilateral small lung nodules can be seen on chest radiographs. As these nodules undergo cystic degeneration,
a cystic or reticular pattern hence predominates in the latter stage of the
disease. The upper and middle zones are
involved to a greater extent than the lung bases, which is related to the
inhalation component of the disease. Lung volumes are usually normal or
increased. Skeletal manifestation of the
disease and complication of pulmonary involvement including pneumothorax or cor
pulmonale are other features on chest radiographs.
On
high resolution CT thorax, there is typically presence of lung nodules together
with cysts of variable wall thickness with upper zone predominance and sparing
of the lung bases. A predominant nodular
pattern can be seen in early stage where predominant thin-wall cysts can be
seen in a latter stage, in keeping with the proposed progression of imaging
abnormalities.
Lymphangiomyomatosis
(LAM) is an important differential diagnosis to pulmonary LCH. The cysts in LCH are usually more variable in
size and wall thickness compared to LAM. They also show upper zone predominance compared with a diffuse
involvement without zonal predominance in LAM. Lung nodule is not a typical
feature in LAM. Another important
distinguishing feature is that LAM occurs almost exclusively in women while LCH
shows a male predominance.
The final diagnosis of LCH usually relies on lung biopsy. Smoking cessation usually leads to stabilization of symptoms in majority of patients. Corticosteroid has also been demonstrated to have beneficial effect in disease stabilization or even clinical and radiological improvement. For patients with advanced pulmonary insufficiency, lung transplant has been performed with success yet recurrence of pulmonary LCH after transplant has been reported in a significant proportion of patients.