Answer of February 2025
For completion of the online quiz, please visit the eHKAM LMS website.
Clinical History:
A 78-year-old lady presenting with acute chest pain radiating to the back.
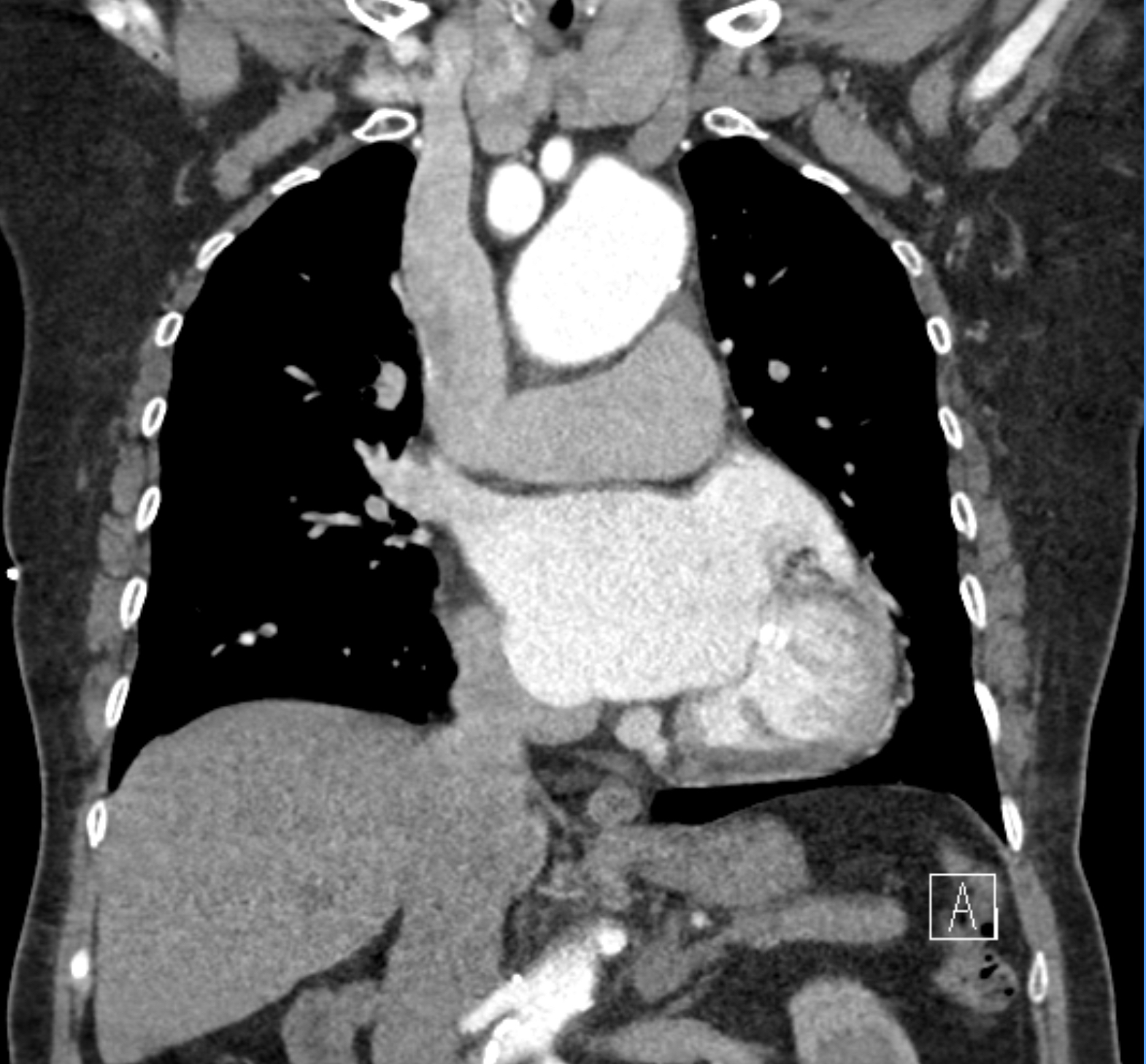
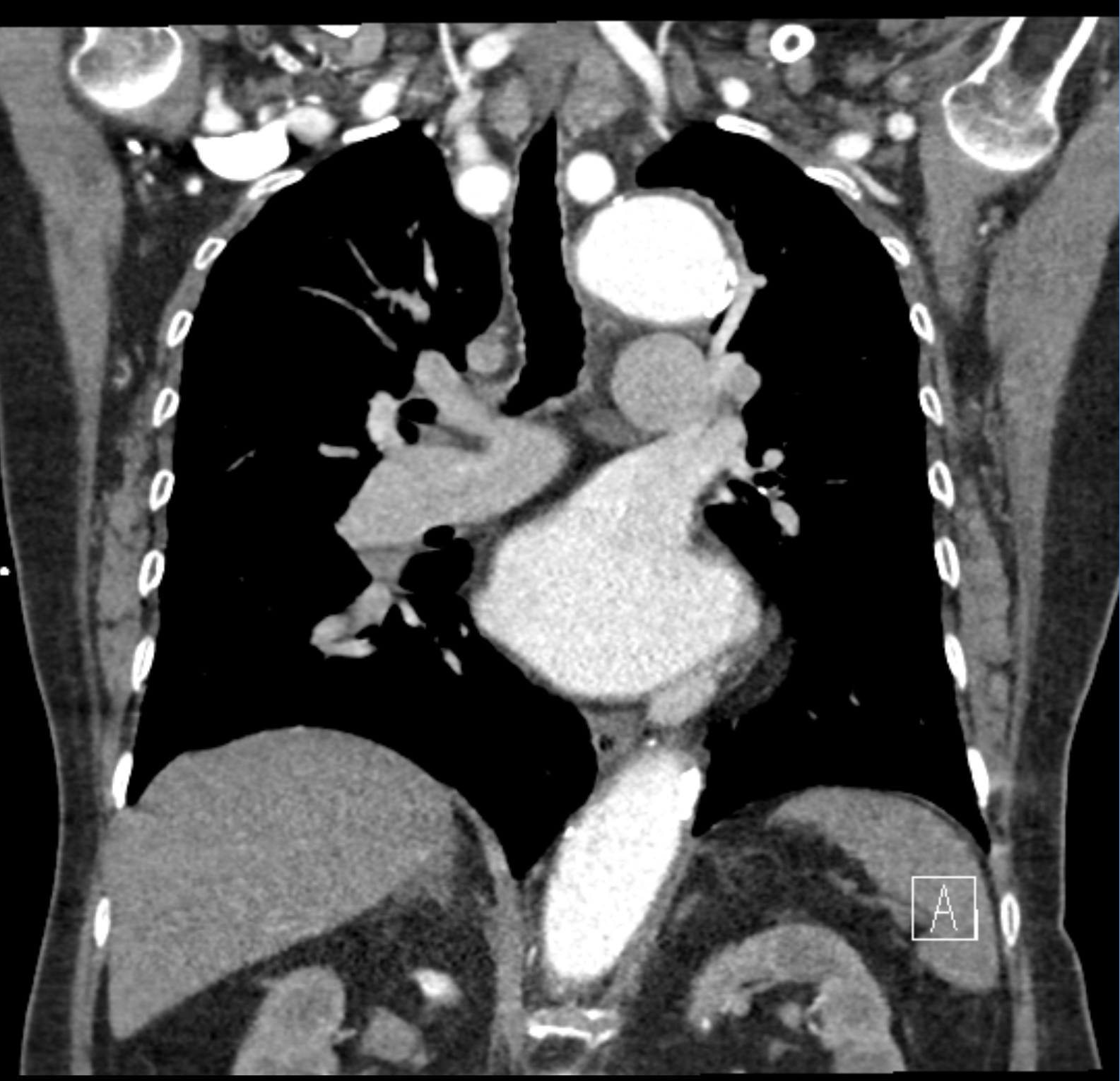
CT Aortogram - coronal
CT Aortogram - coronal
CT Aortogram - coronal
CT Aortogram - coronal
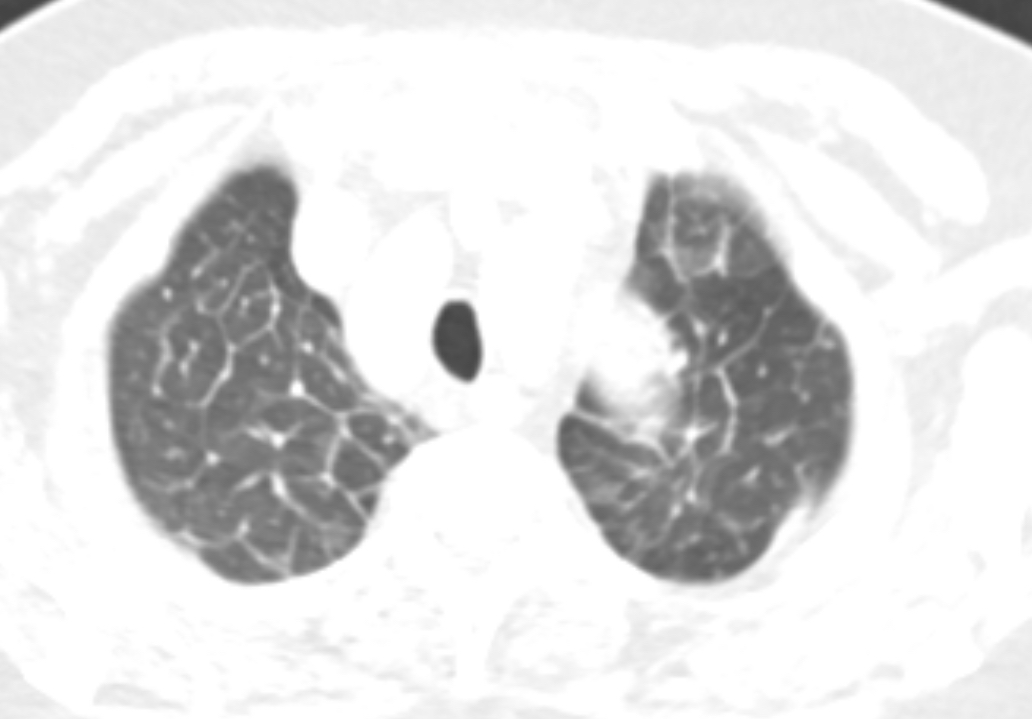
Plain CT (lung window) -
axial
DIAGNOSIS:
Acute inferior myocardial infarction causing cardiogenic pulmonary edema.
DISCUSSION:
Bilateral smooth interlobular septal thickening with upper lobe venous diversion. Dilated azygos vein and wide vascular pedicle width. The combination of findings points towards cardiogenic pulmonary edema. Top differentials would include mitral valve dysfunction and impaired left ventricle function.
The additional finding of hypoenhancing inferior left ventricular wall, along with presenting symptoms of acute chest pain, steers us towards the correct diagnosis of acute inferior myocardial infarction.
This patient was confirmed to have inferior STEMI. Her electrocardiogram shows ST elevation in inferior leads with markedly elevated troponin. She was given thrombolytics with subsequent resolution of chest pain, ST elevation and elevated troponin.
With smooth interlobular septal thickening, there is a wide spectrum of differential diagnoses. The presence of widened vascular pedicle width (superior vena cava to left subclavian artery origin) favors cardiogenic pulmonary edema. This is a useful sign in both XR and CT to differentiate cardiogenic pulmonary edema from other differentials such as non-cardiogenic pulmonary edema and pulmonary interstitial infiltration.
Myocardial infarction is typically diagnosed clinically with electrocardiogram findings and elevated cardiac markers, in the context of acute chest pain. Echocardiogram is also helpful to look for regional wall motion abnormalities corresponding to the vascular territory involved.
However, CT Aortogram may be performed to exclude aortic dissection especially when the pain is described to be radiating towards the back. It is therefore important to recognize the radiological signs of myocardial infarction should such cases appear.
Previous studies have reported up to 89-96% sensitivity and 71-99% specificity for detection of acute myocardial infarcts by first pass CT perfusion studies (ECG-gated).
CT Thoracic Aortogram is essentially a cardiac first pass perfusion study, but without ECG gating. Therefore, we expect to see hypoenhancing myocardium in cases of large territory myocardial infarction. If a delayed sequence (approximately 5 minutes post-contrast injection) were to be obtained, we may observe delayed enhancement of the infarcted myocardium.
Important point to note is to distinguish between acute and old myocardial infarcts. Both will give similar enhancement patterns as described above. However, one may see associated myocardial thinning or subendocardial fat infiltration in chronic cases. It is essential to look at the chronicity of the patient’s presenting complaint.
In cases with ECG-gated CTs, one may be able to identify the site of occlusion. Therefore, knowledge on coronary artery vascular territories is important to make an accurate and comprehensive diagnosis. For inferior myocardial infarcts (as in our patient), we expect to find the site of occlusion at the right coronary artery. As for anterior, apical and lateral myocardial infarcts, we expect to see occlusions at proximal left anterior descending artery, mid left anterior descending artery and left circumflex artery respectively. If 12-lead ECGs are available, it is best practice to make sure that the ECG and radiological localization correlates with each other.
Nitroglycerin is contraindicated for patients with acute inferior myocardial infarcts. The mechanism is thought to be related to right ventricular infarct in right coronary artery occlusion. Nitroglycerin has vasodilating effects on the peripheral veins, thus reducing the preload and causing hypotension. It is reported that approximately 70% of patients with right ventricular involvement will develop hypotensive episode subsequent to nitroglycerin adminiistration.