Answer of January 2025
For completion of the online quiz, please visit the eHKAM LMS website.
Clinical History:
A 81-year-old lady with history of autoimmune disease on long term immunosuppressant presented with insidious onset of decreased general condition for few weeks. Physical examination was unremarkable. She was afebrile. Plain computed tomography (CT) brain showed a space occupying lesion at right basal ganglia with mass effect. Magnetic resonance imaging (MRI) brain with contrast was performed.
Axial plain CT brain
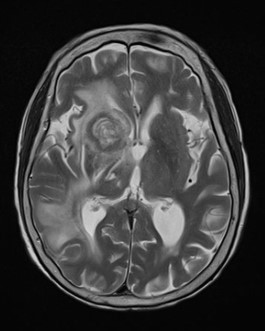
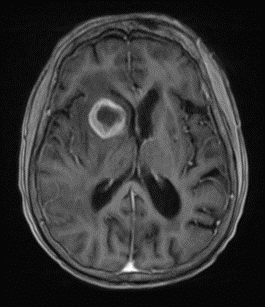
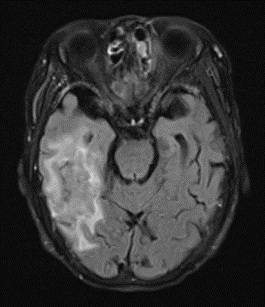
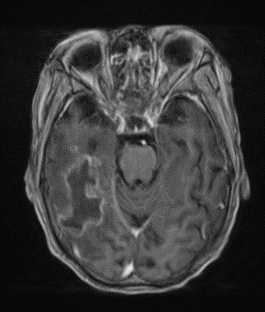
Axial MRI brain T2 weighted sequence
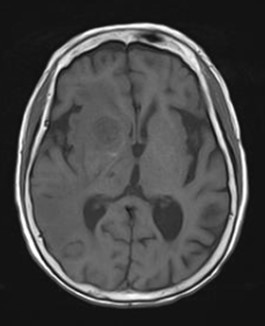
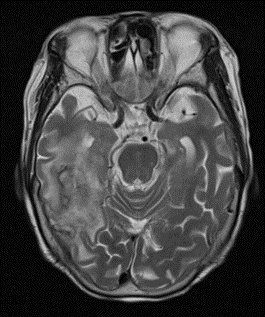
Axial MRI brain T1 weighted sequence
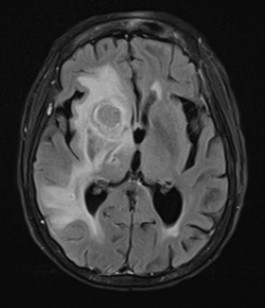
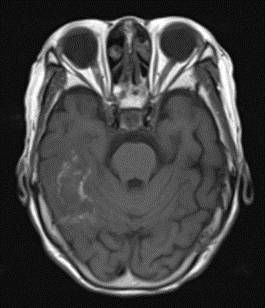
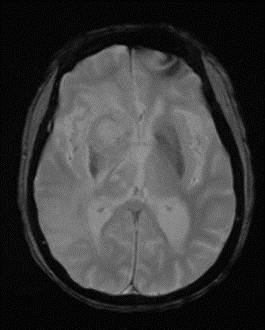
Axial MRI brain Fluid attenuated inversion recovery (FLAIR) sequence with contrast
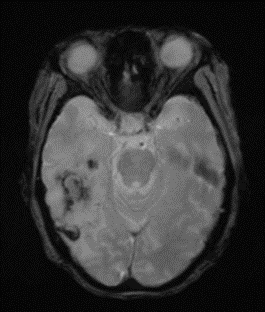
Axial MRI brain gradient echo sequence
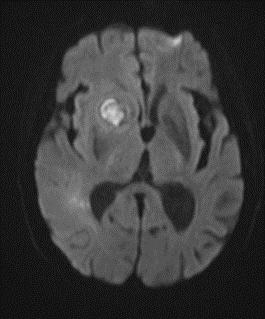
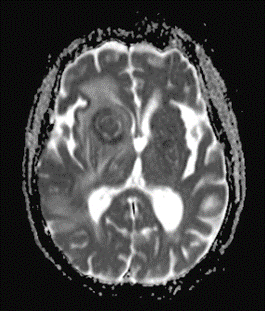
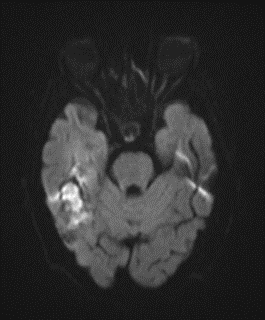
Axial MRI brain diffusion weighted imaging (DWI) sequence, B-value =1000
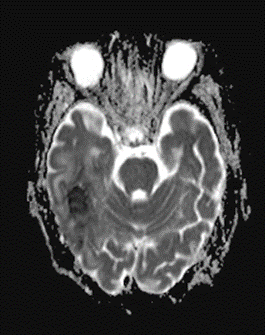
Axial MRI brain apparent diffusion coefficient (ADC) map
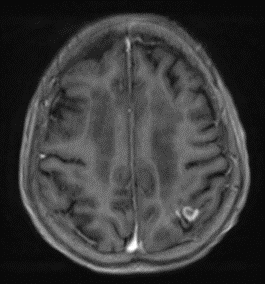
Axial MRI brain T1 weighted sequence with contrast
Axial MRI brain T2 weighted sequence
Axial MRI brain T1 weighted sequence
Axial MRI brain Fluid attenuated inversion recovery (FLAIR) sequence with contrast
Axial MRI brain gradient echo sequence
Axial MRI brain diffusion weighted imaging (DWI) sequence, B-value =1000
Axial MRI brain apparent diffusion coefficient (ADC) map
Axial MRI brain T1 weighted sequence with contrast
Axial MRI brain T1 weighted sequence with contrast
DIAGNOSIS:
Lymphoma - Polymorphic lymphoproliferative disorders in immune deficiency / dysregulation (autoimmune/iatrogenic, WHO HAEM5 classification)
DISCUSSION:
MRI showed multiple intra-axial ring enhancing lesions in right caudate, right temporal lobe and left high parietal lobe. They showed inhomogeneous fluid content with restricted diffusion. The right caudate lesion showed round shape with thick wall (thinner medially), while the right temporal and left high parietal lesions showed irregular thin wall with hemosiderin rim.
In view of uncertain exact nature and mass effect of the intracranial lesions, surgical biopsy and drainage of the right caudate and right temporal lesions was performed. Pus like pinkish fluid was yielded and biopsy samples were obtained. Cytology showed atypical lymphoid infiltrate and histological diagnosis of polymorphic lymphoproliferative disorders in immune deficiency / dysregulation was made.
Microbiology workup was negative. PET/CT showed no evidence of extracranial lymphoma/lymphoproliferative disease. Blood sample showed positive Epstein-Barr virus DNA.
The World Health Organization (WHO) classification of lymphoid tumours has recently been updated to its 5th edition (WHO-HAEM5) in 2022.
In previous classification, immunodeficiency-associated lymphoproliferative disorders were grouped according to the disease background in which they arose, including post-transplantation, HIV infection, primary immunodeficiencies, and other iatrogenic immunodeficiencies. However, as these categories are increasingly recognized to share overlapping pathological features and broader spectrum of immunodeficiency settings is being recognized, WHO-HAEM5 has made major changes to the classification of these disorders. The new classification system consists of a three-part nomenclature, including histological diagnosis, any viral association (e.g. EBV) and immune deficiency/dysregulation setting (e.g. post-transplantation, HIV infection, etc). In the above case, the histological diagnosis of ‘polymorphic lymphoproliferative disorders in immune deficiency / dysregulation (autoimmune/iatrogenic)’ is a new entity in WHO-HAEM5, with histology of polymorphic lymphoproliferative disorders, under setting of immune deficiency / dysregulation related to autoimmune disease or iatrogenic/therapy-related.
As WHO-HAEM5 is only recently introduced, there is lack of literature discussing the specific, if any, radiological features of these lesions. As the change in WHO-HAEM5 is mostly the classification system, the radiological features of these lesions likely resemble that of spectrum of lymphoma, e.g. immunodeficiency-associated central nervous system (CNS) lymphoma in this case.
It is well recognized that radiological features of primary CNS lymphoma can be different between immunocompetent and immunocompromised patients. Immunocompetent primary CNS lymphoma typically demonstrates high cellularity with homogeneous contrast enhancement, located at periventricular white matter, subependymal extension, crossing corpus callosum.
In contrast, immunocompromised primary CNS lymphoma shows more variable and heterogeneous appearance, including multifocal lesions, central necrosis, ring enhancement, microhaemorrhage, lobar and basal ganglia location. These features are present in the above case. However, they can also mimic other pathologies including cerebral abscesses, toxoplasmosis, high grade glioma, etc. Therefore, consideration of the relevant clinical information including medical history, medications, symptoms and signs, are important in narrowing the differential diagnosis.