Answer of December 2024
For completion of the online quiz, please visit the eHKAM LMS website.
Clinical History:
A 72-year-old lady presented with abdominal discomfort, vomiting and loss of appetite for 2 weeks. Oesophago-gastro-duodenoscopy (OGD) found a 5cm submucosal lesion over the posterior greater curve of gastric body with a 5mm overlying clean based ulcer.
CT Abdomen:
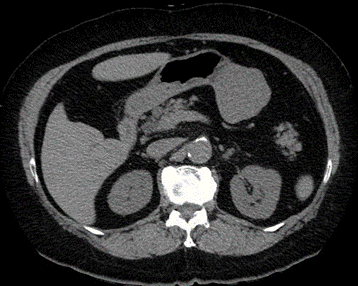
Axial non-contrast CT of abdomen
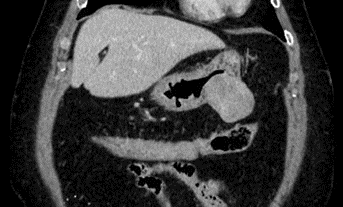
Axial post-contrast CT of abdomen
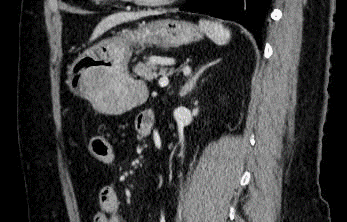
Coronal post-contrast CT of abdomen
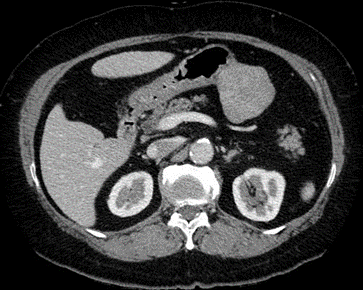
Sagittal post-contrast CT of abdomen
DIAGNOSIS:
Gastric Schwannoma (biopsy proven)
DISCUSSION:
Gastrointestinal schwannomas are rare mesenchymal tumours originating from the neural plexus (Auerbach myenteric plexus) in the gastrointestinal wall. They are most commonly seen in the stomach (60–70%), followed by the colon and rectum. They are more frequently noted between the age of 50 and 80 years with female predominance. Most of them are benign and slow growing, so patients are often asymptomatic and could be found incidentally during gastrointestinal endoscopy, imaging or abdominal surgery. Occasionally patients may present with abdominal discomfort, acid reflux, vomiting and anorexia. When the tumour grows, it could break through the mucosa and results in ulceration and bleeding. Bowel obstruction and intussusception can happen if the tumour is located at the intestine. Malignant transformation of gastrointestinal schwannomas is very rare and only few cases have been reported in literature. Reports have shown that common serum tumor markers were within the normal range, but occasionally increased CA19-9 was observed.
Since gastrointestinal schwannomas mostly occur in the muscularis propria or submucosa, conventional endoscopic tissue biopsy usually only shows chronic inflammatory manifestations of the mucosa but not able to give a definite histopathological diagnosis. Endoscopic ultrasound-guided biopsy is recommended as a routine examination method to confirm the preoperative diagnosis of submucosal tumours . Positivity for S-100 protein in histology is the gold standard for diagnosing gastrointestinal schwannomas.
On abdominal computed tomography (CT) scans, gastrointestinal schwannomas appear as well-defined, round, mural masses with homogeneous attenuation arising from the wall of the gastrointestinal tract. Common differential diagnosis included gastrointestinal stromal tumours (GISTs) and leiomyomas. As compared with GISTs, gastrointestinal schwannomas rarely present with features of hemorrhage, necrosis and cystic changes on CT. They are also less likely to result in ascites and malignant metastasis as compared with other malignant tumours. The tumours on magnetic resonance imaging (MRI) would demonstrate low or intermediate T1-weighted signal intensity, and high T2-weighted signal intensity. 18FDG- Positron Emission Tomography (PET) may be of limited value as a preoperative diagnostic technique for the assessment of gastrointestinal schwannomas but they are used to detect recurrence and metastasis of the malignant forms.
Benign gastrointestinal schwannomas carry a good prognosis. Complete surgical removal of the tumour is the main method of treatment in symptomatic patients or to avoid future complications.