Answer of November 2024
For completion of the online quiz, please visit the eHKAM LMS website.
Clinical History:
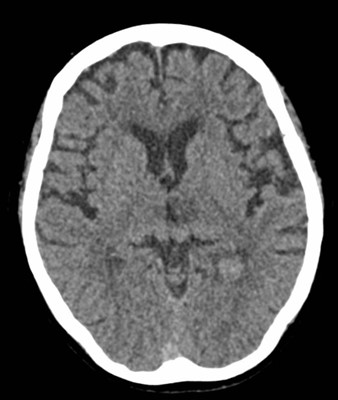
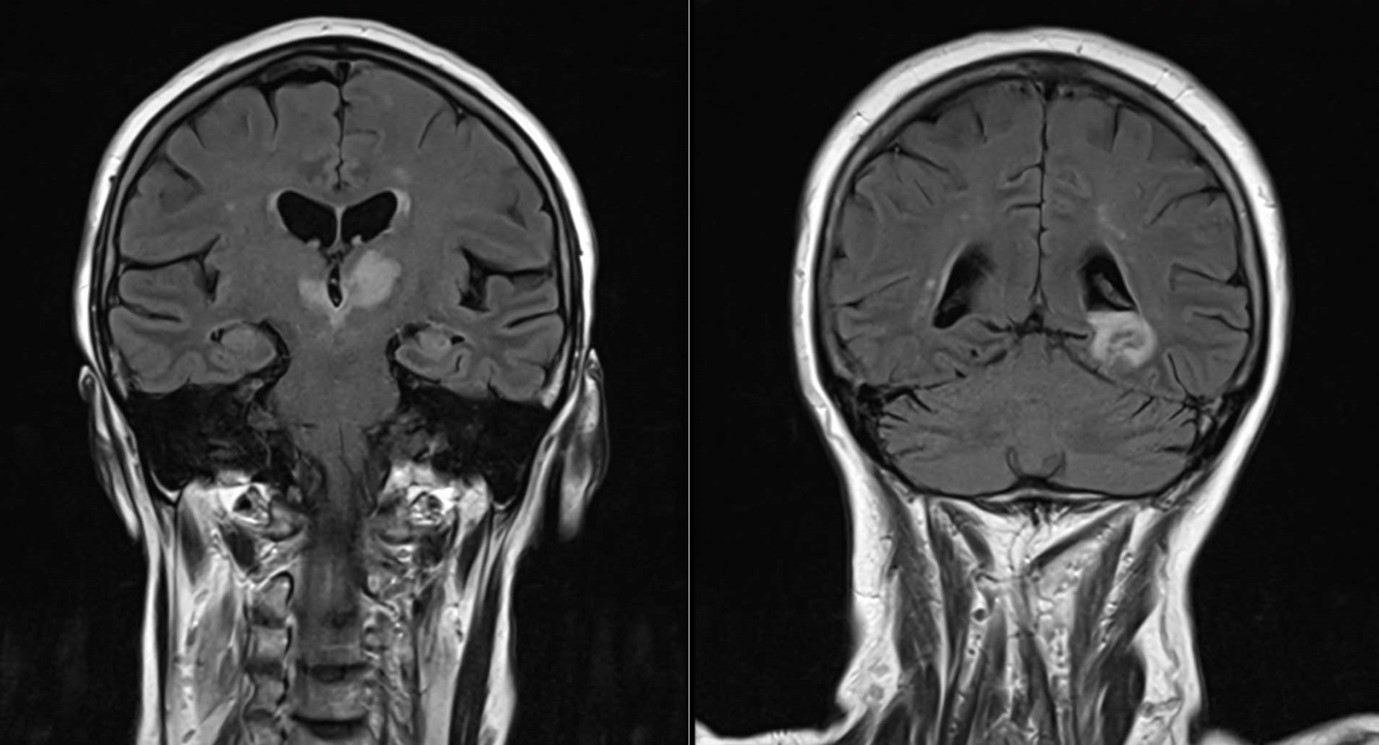
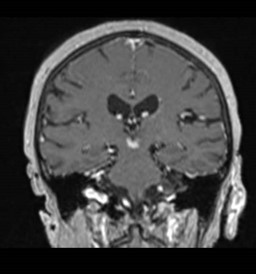
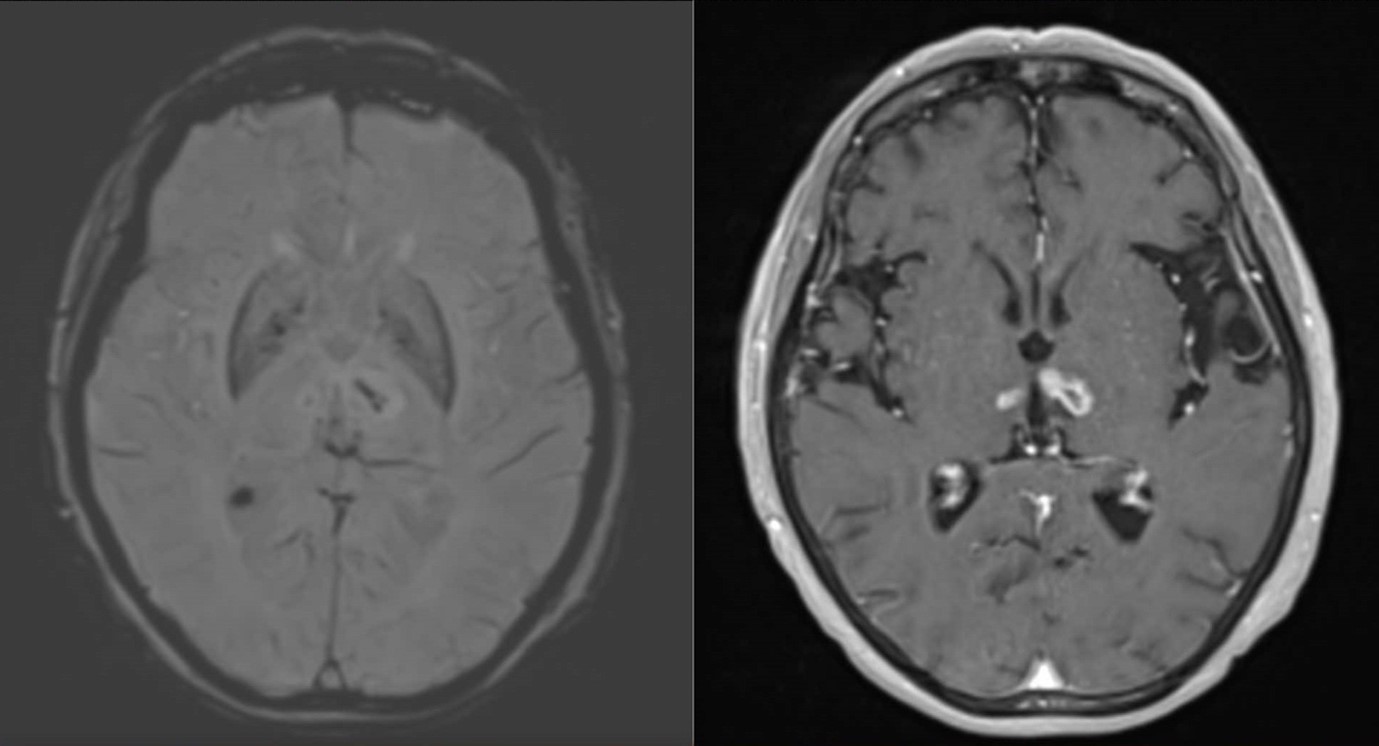
A 71-year-old woman presented with low-grade fever, dizziness and fall, which was followed by acute onset of bilateral complete ptosis and bilateral internuclear opthalmoplegia. Plain CT brain and contrast-enhanced MRI brain were performed.
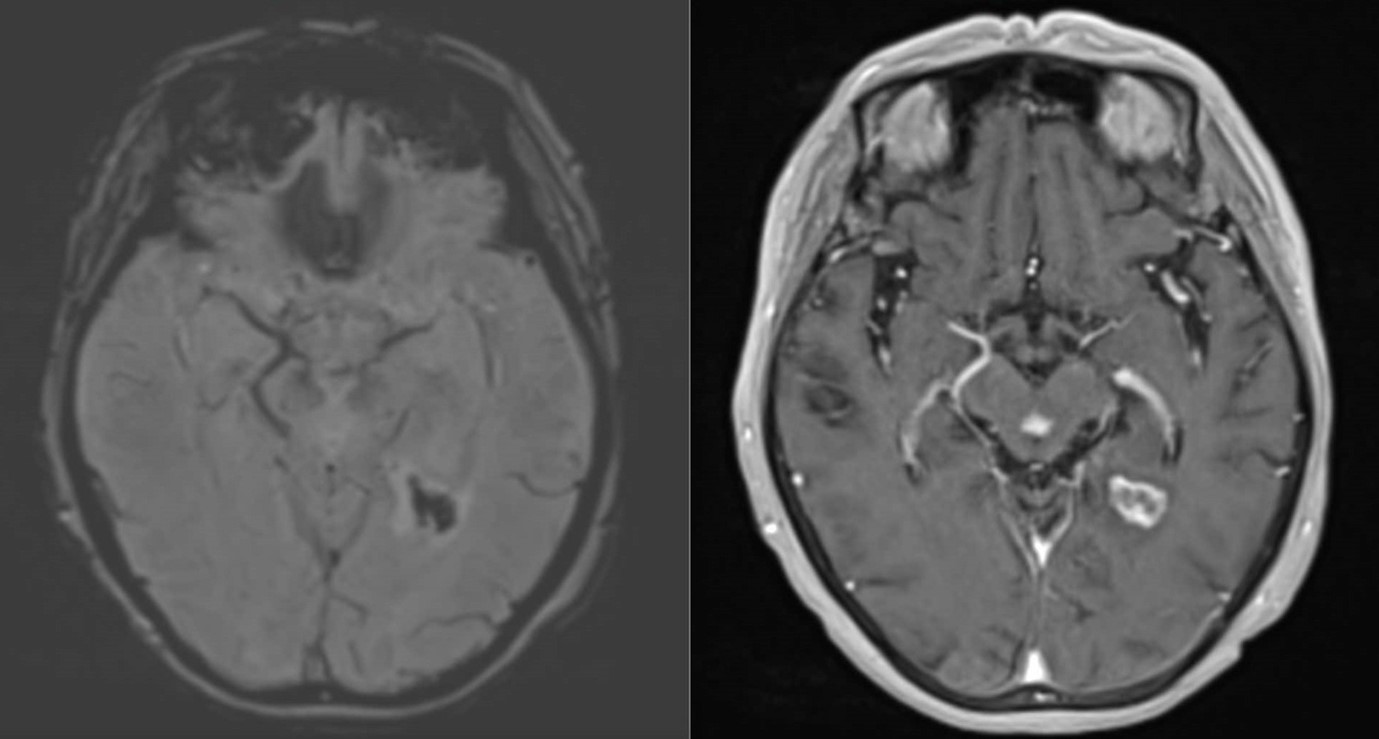
CT brain:
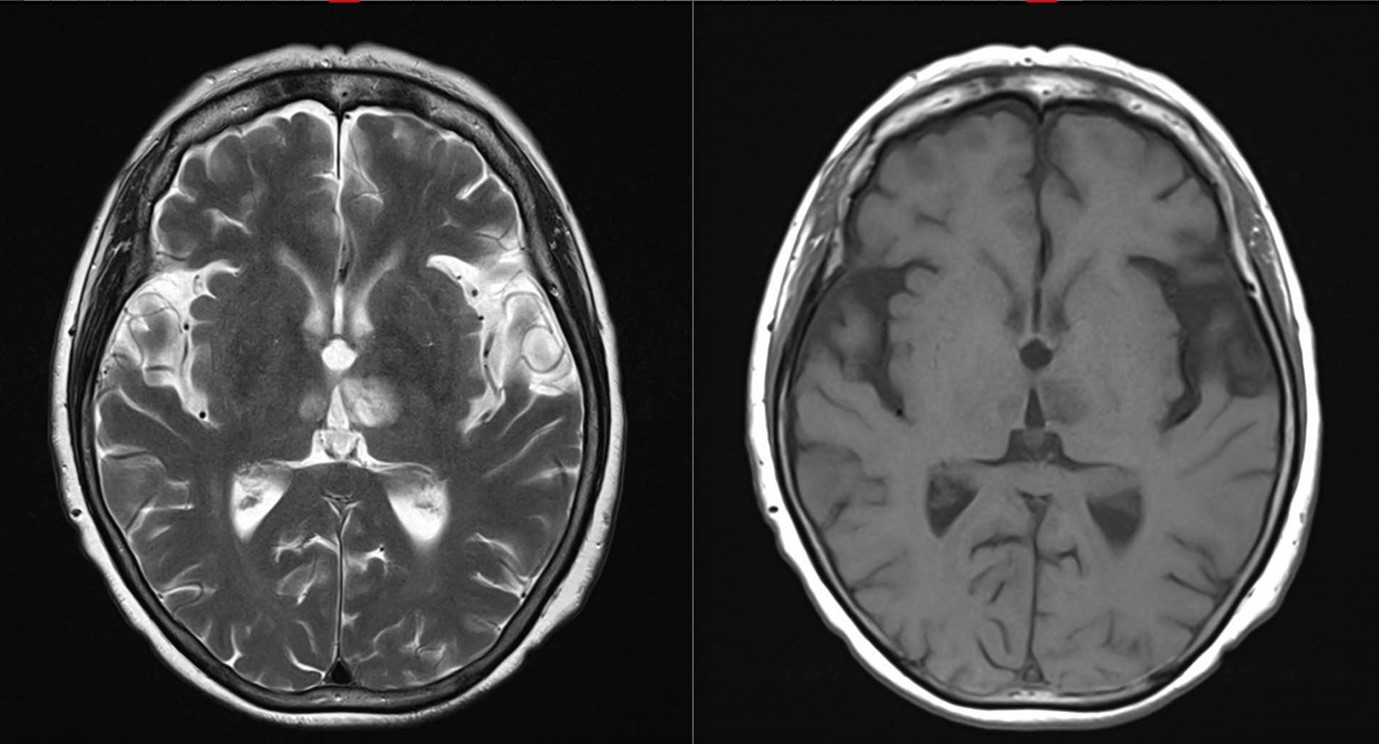
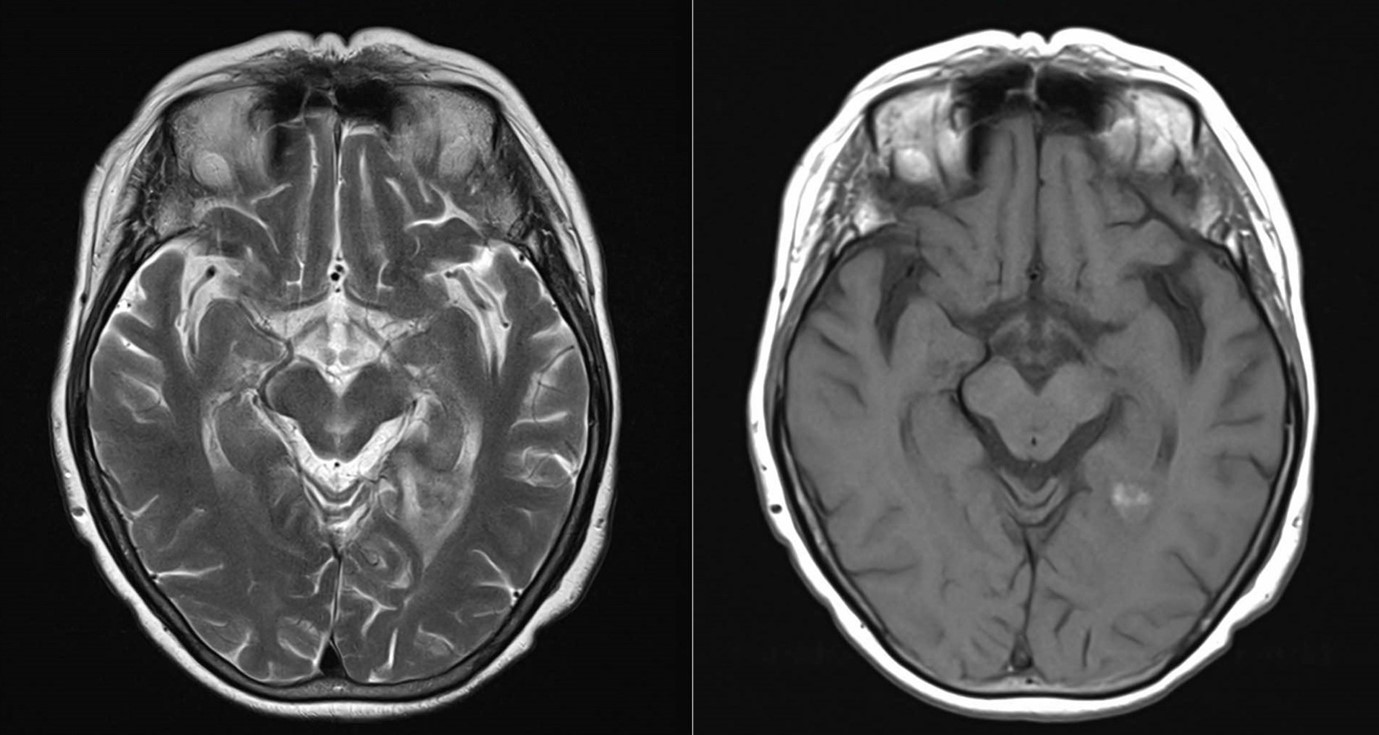
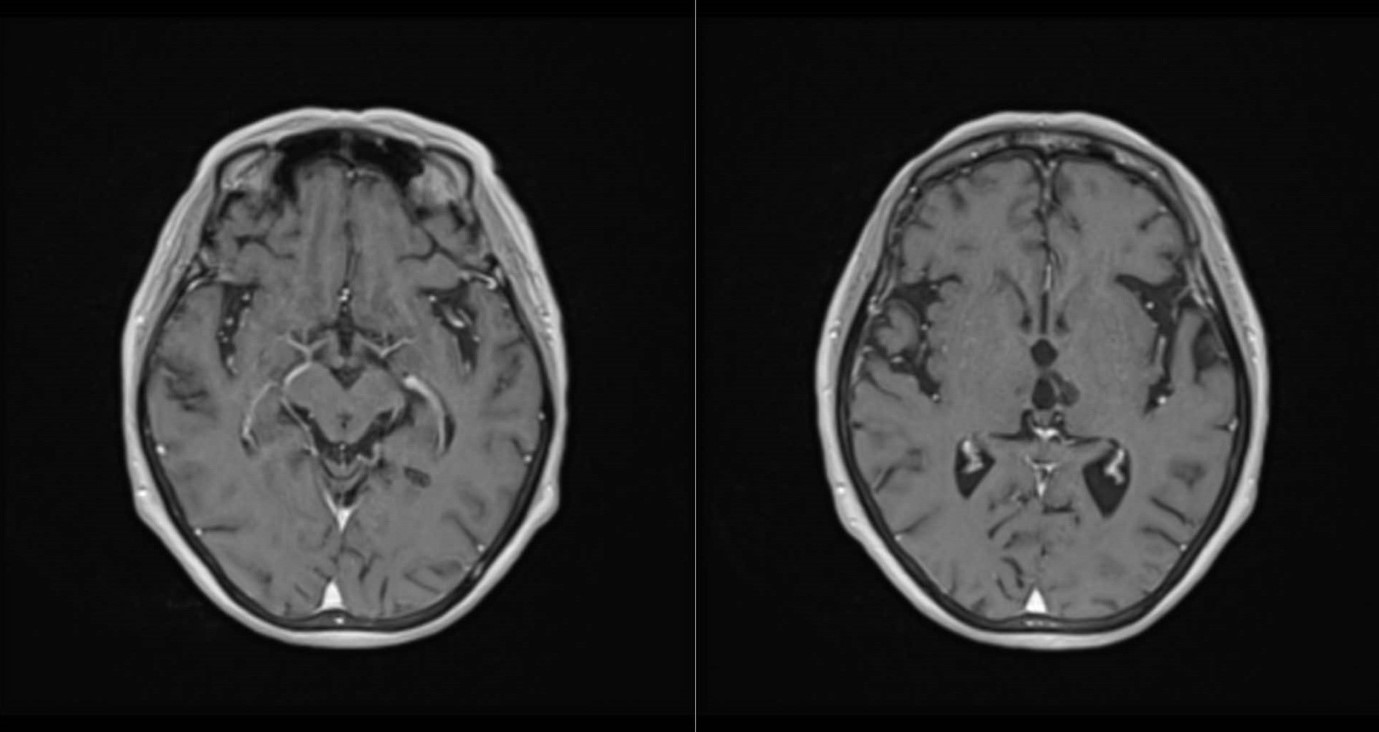
MRI brain:
DIAGNOSIS:
Artery of Percheron infarction.
DISCUSSION:
The differential diagnoses for bilateral thalamic lesions are broad, including neoplastic, vascular, infectious, metabolic and congenital disorders. We can prioritize different diagnoses based on MR signal characteristics, calcifications, precise position within the thalamus, symmetry/asymmetry, the presence of concurrent extra-thalamic lesions and so on. It is also essential to correlate with clinical and laboratory findings and follow-up imaging is helpful.
Bilateral thalamic arterial infarcts are actually uncommon. The thalami are supplied by both anterior (anteroinferior thalami) and posterior (medial thalami) circulation, but several variations occur. The artery of Percheron, a variant, is a solitary arterial trunk arising from the proximal segment of the posterior cerebral artery and supplying the paramedian thalami and rostral midbrain bilaterally. Occlusion causes bilateral thalamic infarction as in this case, which could result in asymmetrical bithalamic involvement. The regression of the lesions in the follow-up MRI with encephalomalacia changes confirms the diagnosis. The rim enhancement of the infarcted tissue could persist for weeks to months and the presence of hemosiderin could be also present due to microhaemorrhage or haemorrhagic transformation.
The regression of the lesions exclude neoplastic cause for this patients. Cerebral metastases have a predilection for the vascular border zone and grey-white matter junction, and less frequently involve the deeper brain. Primary CNS lymphoma tends to involve the white matter with restricted diffusion, although it could not be properly assessed due to presence of hemosiderin. Haemorrhagic transformation is rarer in primary CNS lymphoma except for immunocompromised patients.
Wernicke encephalopathy usually presents as increased T2 signals in bilateral thalami predominately at the dorsomedial aspects, and could involve the mammillary bodies, tectal plate and peri-aqueductal grey matter. However, in this case the dorsomedial thalami are rather spared.
Creutzfeldt-Jakob disease most commonly involves the cerebral cortex and could also involve the deep grey matter, which characteristically shows the hockey stick sign and/or pulvinar sign of thalamic involvement. Again the medial aspect of the dorsomedial thalami are rather spared in this case.