Answer of August 2024
For completion of the online quiz, please visit the eHKAM LMS website.
Clinical History:
A 14-year-old male presented with persistent right ankle pain 3 weeks post-injury.
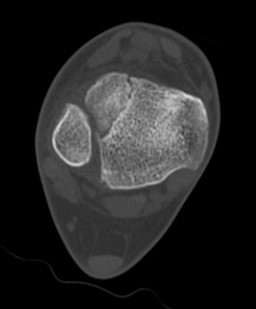
X-ray of bilateral ankles
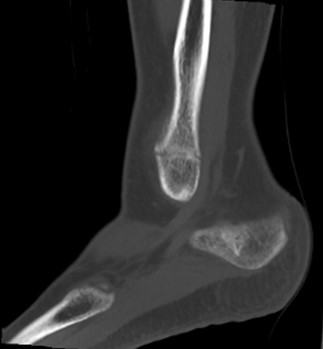
CT of right ankle
DIAGNOSIS:
Right distal tibial Tillaux fracture and Salter-Harris type I fracture of distal fibula.
FINDINGS:
X-ray showed widening of physis at right distal tibia with apparent lucency at its epiphysis. Increased opacities at lateral aspect of right distal tibia, can be smooth periosteal reaction due to healing process.
Cortical irregularity with widening of physis at right distal fibula, suspicious of fracture with physeal injury. Mild soft tissue swelling at right ankle.
Computed tomography (CT) of right ankle showed distal tibial fracture traveling horizontally through the physis and extending vertically through the epiphysis, compatible with Tillaux fracture. Smooth periosteal reaction along lateral aspect of distal tibia. Fracture through physis of distal fibula, in keeping with Salter-Harris type I fracture.
DISCUSSION:
Juvenile Tillaux fracture of distal tibia typically presents in adolescents approaching skeletal maturity at around 12 to 15 years old, with higher incidence rate in girls who present at a younger age due to earlier physeal fusion. It accounts for 3-5% of pediatric ankle fractures.
Characteristic sequence of distal tibial physeal closure starting centrally, progressing anteromedial and posteriorly, and ending laterally over a transitional period of about 18 months predisposes the lateral physis to this type of injury. Anterolateral corner of distal tibial epiphysis is avulsed by anterior tibiofibular ligament during external rotation injury of foot in supination. This results in horizontal fracture along the unfused physis until meeting its fused portion, where subsequent vertical extension through the epiphysis occurs, i.e. Salter-Harris type III fracture.
X-ray of bilateral ankles with AP, lateral and Mortise views are considered first line investigations in adolescent patients with suspected ankle fracture. Contralateral ankle X-ray aids assessment of physeal plate status and offers comparison to enable detection of subtle physeal injuries.
Further workup with CT helps to delineate fracture pattern, degree of displacement and articular congruency. Fracture with less than 2mm displacement can be treated conservatively with closed reduction and casting. Operative management is considered when there is more than 2mm displacement to prevent early arthritis, chronic ankle pain and stiffness. Significant growth disturbance is rare in this group of patients with near complete fusion of growth plates.
In summary, subtle physeal separation in juvenile Tillaux fracture may be difficult to detect on plain X-ray. A high index of suspicion is important to prevent long term consequences. CT should be recommended in suspected cases.