Answer of July 2024
For completion of the online quiz, please visit the eHKAM LMS website.
Clinical History:
A 9-year-old boy with a history of repeated vomiting since 5 years old, each time lasting for 4-7 days. This time he was admitted for repeated vomiting of greenish fluid for 10 days.
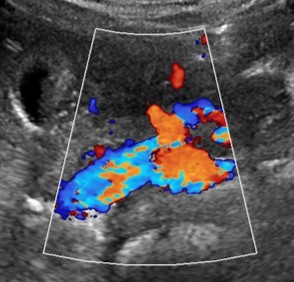
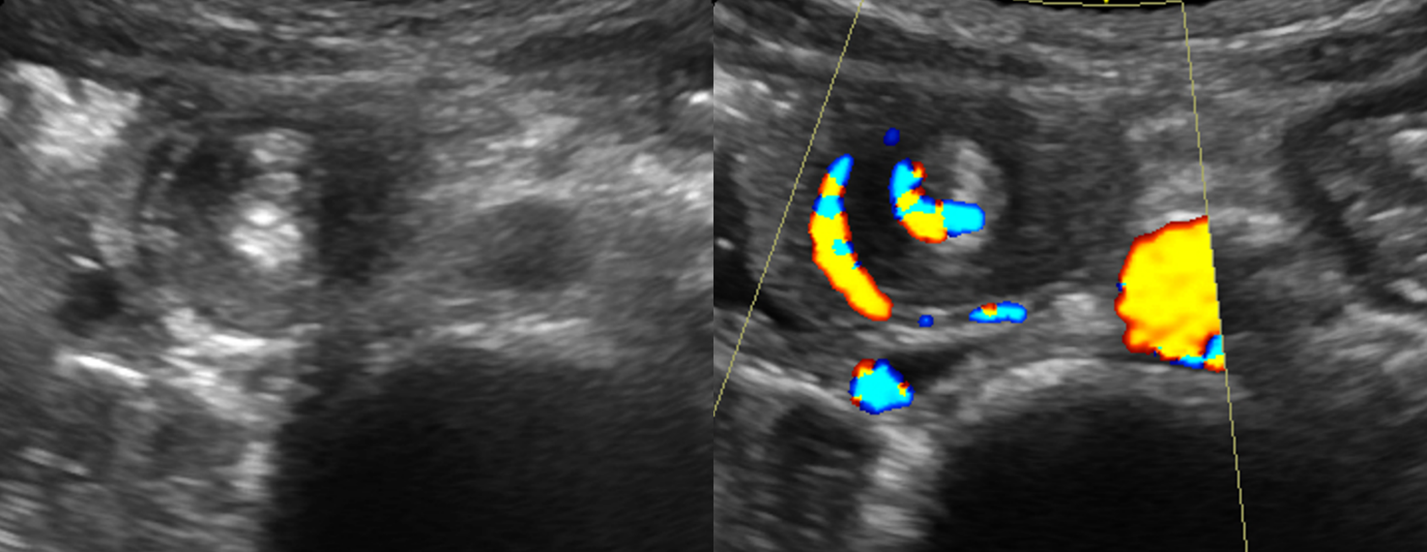
US of the upper abdomen
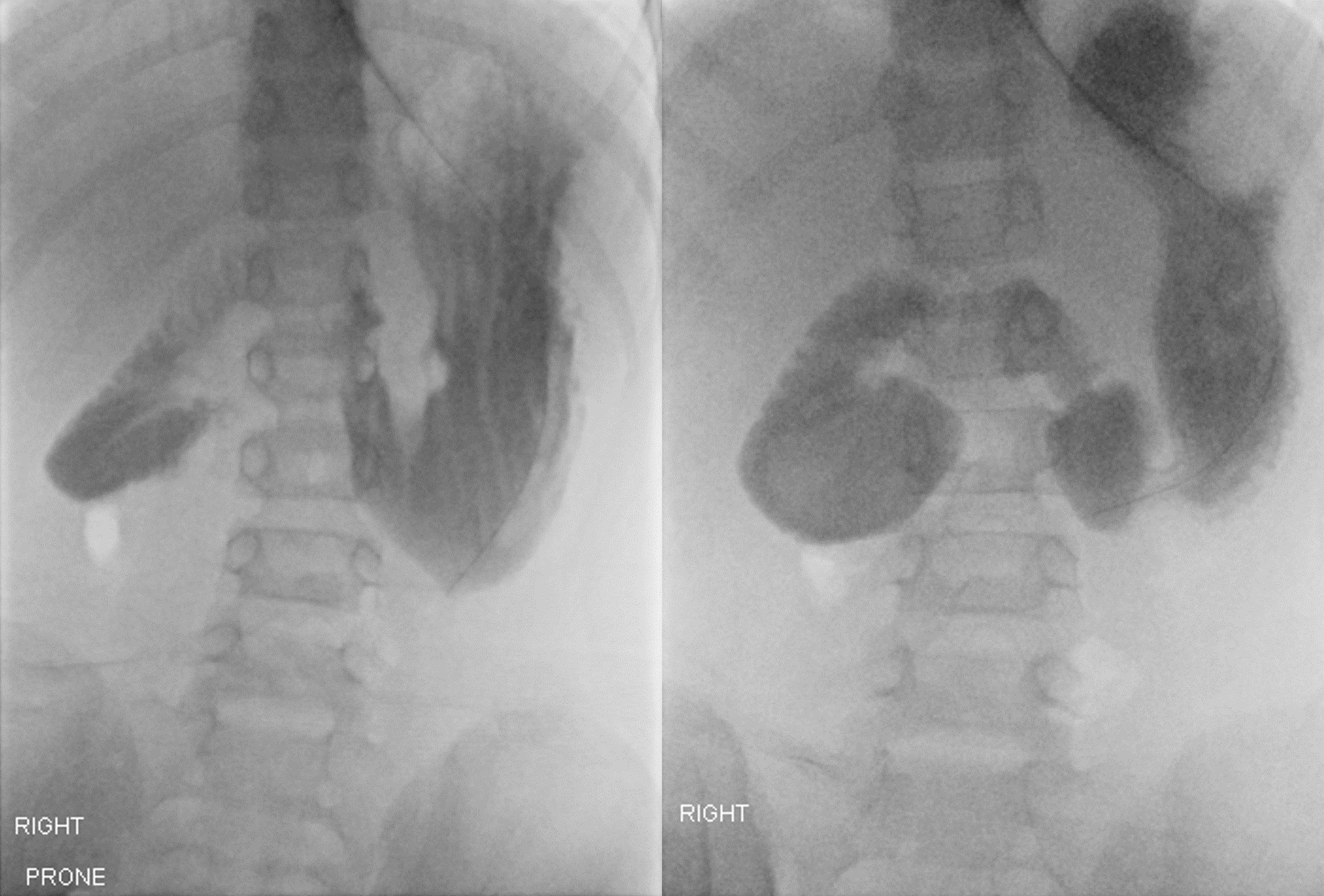
Fluoroscopic UGI contrast series
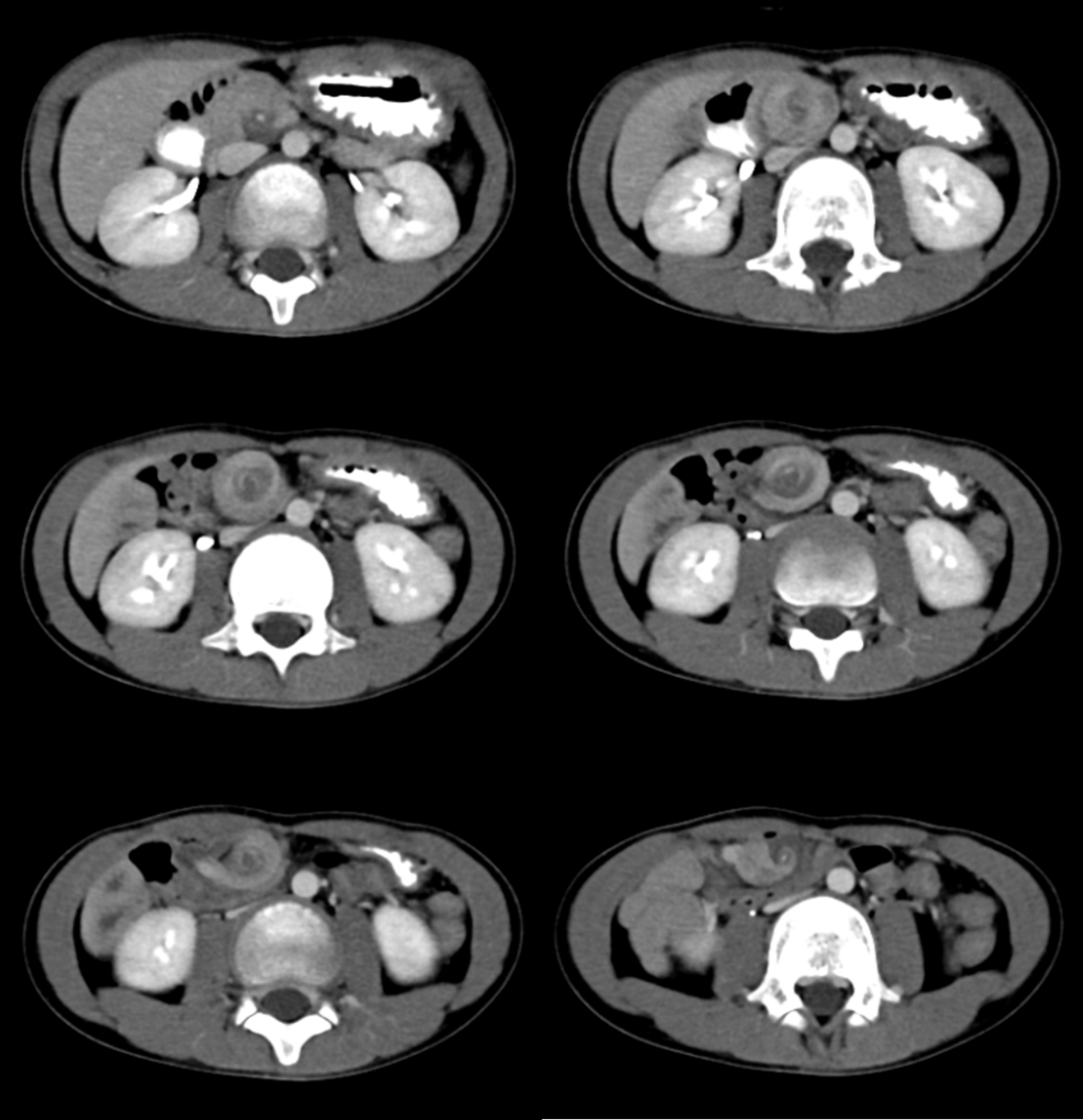
Contrast CT abdomen and pelvis
DIAGNOSIS:
Midgut malrotation and volvulus
FINDINGS:
Ultrasound (US) of the abdomen showed inverted SMA/SMV relationship. The stomach and proximal duodenum are dilated, with abrupt change in calibre at D2/3 level. The D3 duodenum descends along the right sided abdomen without crossing midline, and enters a loop of bowel with a swirling appearance.
Fluoroscopic upper gastrointestinal (UGI) contrast series was performed, which showed upholding of contrast at D3 duodenum with beaking. Ineffective peristalsis with retrograde flow of contrast were observed. No further contrast advancement despite positional manoeuvres or delayed imaging.
Contrast computed tomography (CT) of the abdomen confirmed midgut malrotation with volvulus. Superior mesenteric artery (SMA) and superior mesenteric vein (SMV) within the twisted mesentery were attenuated. Bowel mucosal enhancement was preserved. There was no pneumoperitoneum.
Subsequent surgery confirmed midgut malrotation complicated with volvulus of 900 degrees.
DISCUSSION:
Midgut malrotation is a congenital anomaly where there is abnormal rotation and fixation of the bowel during embryogenesis. This results in a narrow mesenteric root attachment where the bowel may twist upon and cause midgut volvulus. It occurs most commonly during infancy with bilious vomiting, and occasionally presents in older patients with chronic symptoms. Midgut volvulus in association with malrotation is a paediatric surgical emergency, requiring prompt and accurate diagnosis to avoid bowel ischemia, thus reducing morbidity and mortality.
UGI series and US are usually first-line imaging modalities for suspected midgut malrotation and volvulus.
Midgut malrotation can be diagnosed on UGI series by determining the location of duodenojejunal (DJ) junction. Normal position of the DJ junction should be to the left of the left sided vertebral body pedicle at the level of the duodenal bulb on frontal view. In malrotation, the DJ junction fails to cross midline to the left of the left-sided vertebral body pedicle and lie inferior to the duodenal bulb on frontal view. On lateral view, D2 and D3 segments of the duodenum do not reach the retroperitoneum. Spiral appearance of distal duodenum and proximal jejunum (known as corkscrew sign) suggests midgut volvulus. In complete obstruction, beaking of the proximal small bowel may be observed.
In midgut malrotation, US may detect inversion of SMA/SMV relationship seen as SMV located anterior to or to the left of the SMA-aorta axis, and an intraperitoneal course of D3 segment of duodenum anterior to the SMA. Presence of clockwise swirl of the SMV and bowel loop around the SMA (known as whirlpool sign) with dilated duodenum and stomach proximal to the obstruction site on US suggest midgut volvulus.
CT can be considered in atypical or uncertain cases. Presence of whirlpool sign with twisted mesentery, inverted SMA/SMV relationship and bowel obstruction confirm the diagnosis. Complications such as bowel ischemia and pneumoperitoneum can also be assessed.