Answer of April 2024
For completion of the online quiz, please visit the eHKAM LMS website.
Clinical History:
36/F with low back pain.
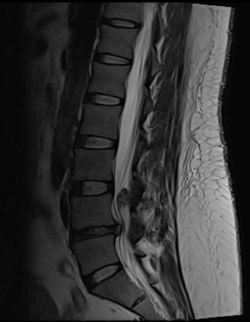
Index MRI, T2W
Index MRI, T1W
Index MRI
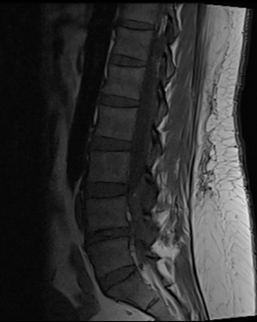
MRI after 3 months (no surgery)
T2W
MRI after 3 months (no surgery)
T1W
MRI after 3 months (no surgery)
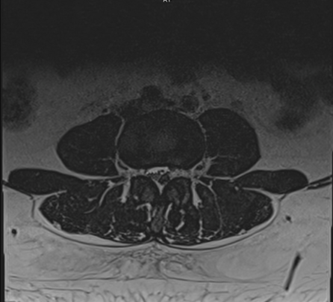
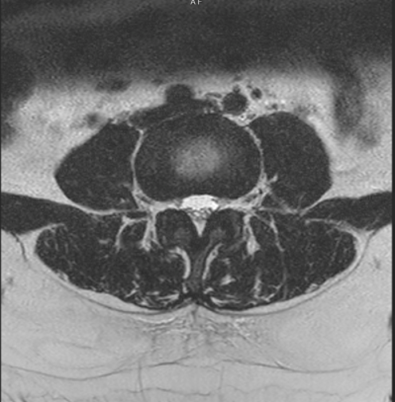
T2W axial at L4 level
DIAGNOSIS
Sequestrated disc fragment
DISCUSSION
Posterior epidural migration of a sequestrated lumbar disc fragment is a relatively rare condition, with most reported cases involving the lumbar region. The migration of the disc fragment to the epidural space usually occurs in a posterior and posterolateral direction to the anterior epidural space. However, migration posterior to the anterior epidural space is uncommon. In the literature, there have been only a few reported cases of posterior migration, and most of them have been observed in the lumbar region.
Imaging plays a crucial role in the diagnosis of this condition. Myelography can demonstrate a complete block of the contrast medium at the level of disc herniation or sequestration, but it cannot provide detailed information about the nature of the compression. CT or CT myelography findings are inconclusive in recognizing the extradural migrated fragment as a mass compressing the dural sac. Therefore, the differential diagnosis may include other pathologies such as tumors (intradural extramedullary), synovial cysts, dural abscesses, or hematomas.
Magnetic resonance imaging (MRI), particularly with gadolinium administration, is considered the method of choice for diagnosis. Sequestrated fragments typically exhibit low signal intensity on T1-weighted images and high to intermediate signal intensity on T2-weighted images relative to the degenerated disc of origin. The high signal intensity on T2-weighted images may be due to either the higher water content of the herniated material compared to an intact disc or a reparative process leading to transient water gain. Gadolinium-enhanced MRI often shows peripheral contrast enhancement around the sequestrated tissue, indicating an inflammatory response with granulation tissue and newly formed vessels.
To differentiate posterior epidural disc migration from other pathologies, it is important to consider the characteristic imaging features. Tumors usually enhance on gadolinium-enhanced MR images, while synovial cysts have a distinct MR imaging signal intensity and are associated with the facet joint. Epidural abscesses typically present as masses with specific imaging characteristics, including hypointensity on T1-weighted images, hyperintensity on T2-weighted images, and rim enhancement. Hematomas, on the other hand, often display heterogenicity, isointensity or hyperintensity on T1-weighted images, no enhancement, and are associated with a history of trauma.
The management of posterior epidural migration of a sequestrated lumbar disc fragment is a topic of debate, and both conservative therapy and early surgical treatment have been proposed as management options. Early surgical treatment has been proposed as the management of choice to prevent further severe neurological deficits. On the other hands, spontaneous regression of the herniated disc has been reported, for example in this case, the patient did not undergo any surgical management and the herniated disc resolved.
In conclusion, posterior epidural migration of a sequestrated lumbar disc fragment is a rare condition that requires accurate diagnosis to avoid unnecessary surgery. MRI with gadolinium administration is the preferred imaging modality for diagnosis, and careful consideration of the imaging features is crucial to differentiate this condition from other pathologies.