Answer of February 2024
For completion of the online quiz, please visit the eHKAM LMS website.
Clinical History:
A 53-year-old woman with right knee pain. Bone scan, XR and MRI of right knee were performed.
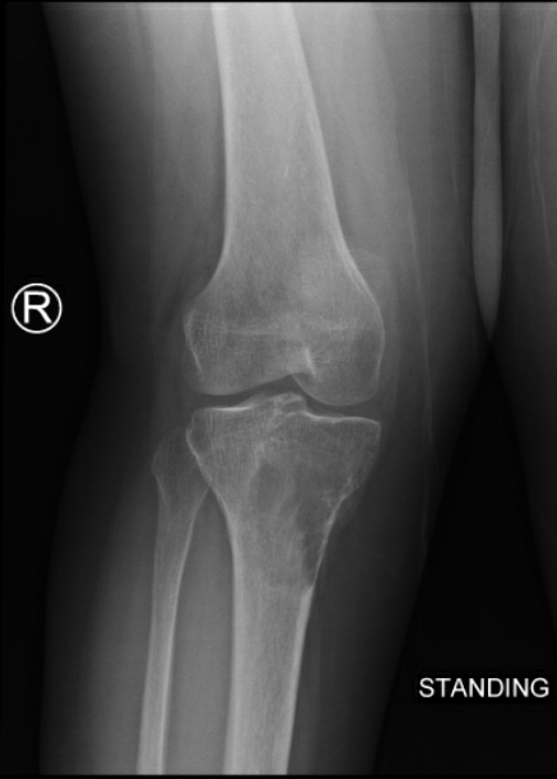
XR of right knee
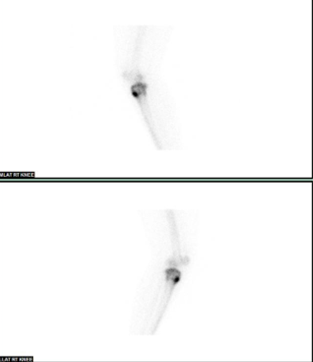
Bone scan
Whole body anterior and posterior views
Right knee lateral views
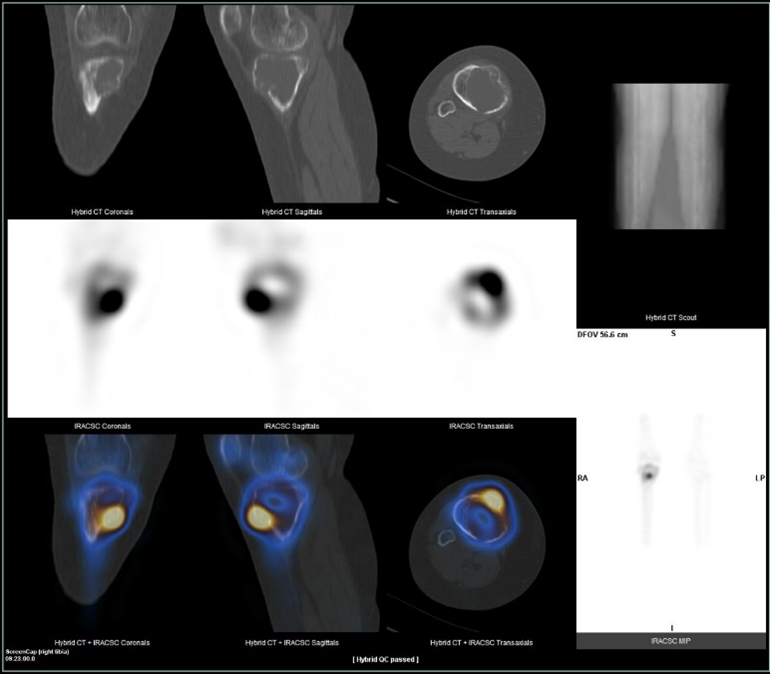
SPECT/CT (coronal, sagittal, transaxial)
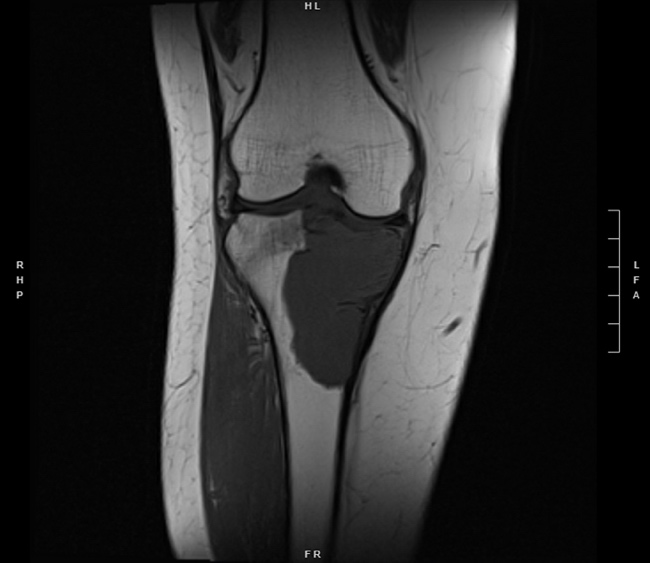
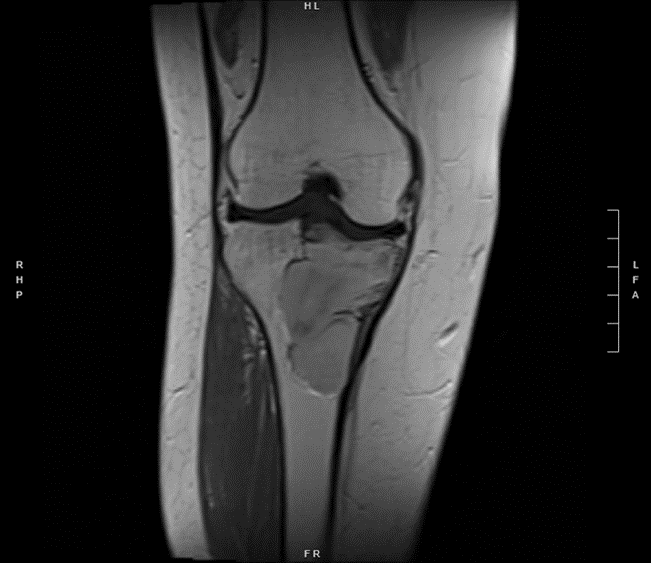
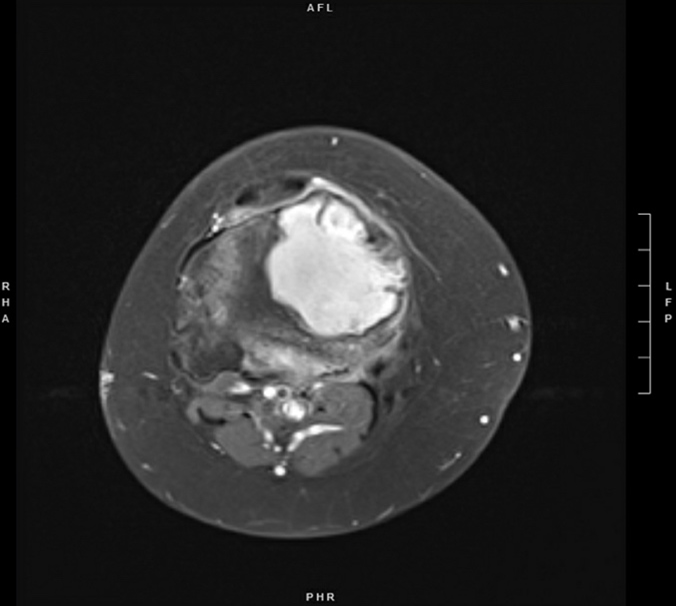
MRI of right knee
T1W
T1W+C
T2W_DIXON_W
T1W+C_DIXON_W
DIAGNOSIS
Giant cell tumour
FINDINGS
Radiograph of right knee shows a slightly ill-defined lytic lesion at the proximal tibia epi-metaphyseal region. No pathological fracture or periosteal reaction.
Bone scan shows abnormal uptake in right proximal tibia, with increased uptake around the periphery and central photopenia. SPECT/CT reveals a lytic bone lesion in right proximal tibia extending to the articular surface with cortical thinning. No peri-lesional soft tissue or collection. No abnormal uptake in rest of skeleton.
MRI of the right knee shows a well circumscribed lobulated lesion eccentrically occupying the proximal right tibia, involves the epiphysis and metadiaphysis region, and extends to the articular surface of the tibial plateau. It is T1 isointense and T2 hyperintense with relatively homogenous contrast enhancement. Mild reactive edematous changes is detected at the adjacent tibial bone marrow.
DISCUSSION
Giant cell tumour (GCT) is generally considered as a benign tumour, but it may demonstrate locally aggressive features and rarely become metastatic. Most GCT occurs in patients between 30 and 50 years of age. Most common locations include distal femur, proximal tibia and distal radius.
The typical appearance on radiograph is a lytic lesion with a well-defined non-sclerotic margin that is eccentrically located at the epiphysis and abuts the articular surface, and occurs in patients with closed physes. For lesions located at the epiphysis, there is limited differential diagnosis. In young patients the considerations are mainly chondroblastoma or infection. In matured skeleton, the differential diagnosis includes giant cell tumour, geode or metastases.
On bone scan, there is typically increased peripheral uptake with a central photopenic area in GCT, known as “doughnut sign”. If triphasic bone scan is performed, increased uptake would be found in all three phases. This uptake pattern is attributable to reactive bone formation around the periphery and increased blood flow in GCT. The photopenic centre could be explained by the predominant osteoclast-like giant cells content with little or no bone formation, as well as presence of necrosis, haemorrhage or aneurysmal change. However, “doughnut sign” is not specific to GCT and can also be seen in other tumours such as aneurysmal bone cyst, telangiectatic osteosarcoma and chondrosarcoma. In addition to assessment of local tumour, bone scan is sensitive in detecting multicentric disease, which is uncommon and tends to involve extremities in young patients.
MRI findings are non-specific, usually intermediate signal or hypointense on T1W images, hyperintense on fluid sensitive sequences, and demonstrates contrast enhancement. It may demonstrate aggressive features such as cortical thinning, periosteal reaction or associated soft tissue mass. Fluid-fluid levels may be seen with secondary formation of an aneurysmal bone cyst (ABC). GCT and ABC may mimic each other and one of the differentiating features is the presence of enhancing soft tissue component, which may be present in GCT but should not be present in primary ABC.
Lung metastases has been reported in about 1-6% of patients with GCT. Although lung metastases are commonly resected, most pulmonary lesions are histologically benign and often have an indolent course and may not require treatment. In <10% cases of GCT may also undergo malignant transformation into sarcoma, which has a poor prognosis.
Treatment of GCT should be discussed at a multidisciplinary meeting. Classical treatment is curettage with cement placement. Denosumab has been used as neoadjuvant therapy or in benign metastasising disease. Recurrence rate is around 15-25%.