Answer of November 2023
For completion of the online quiz, please visit the eHKAM LMS website.
Clinical History:
A middle-aged woman with history of renal transplantation on cyclosporin A presented with a painless progressive swelling at the right vulva. Physical examination demonstrated a soft lump at the right vulva. She was also found to have bilateral axillary ectopic breast tissues and giant fibroadenomas after renal transplantation. Ultrasound and plain MRI of the concerned region were performed subsequently.
Ultrasound of Right Vulva
Doppler ultrasound of Right Vulva
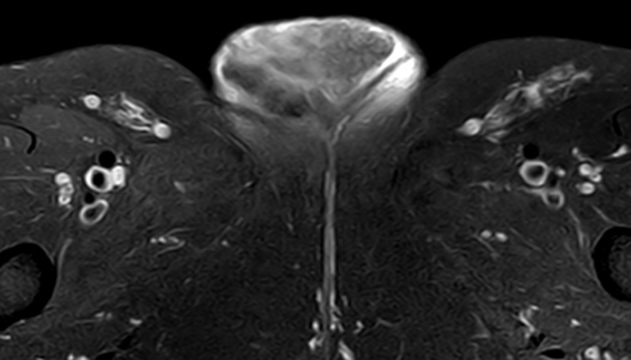
Axial fat -suppressed T2-weighted MR image

Coronal T1-weighted MR image
DIAGNOSIS
Vulvar ectopic breast tissue
IMAGING FINDING
US image of the right vulva shows a soft tissue mass confined to subcutaneous layer with no deep extension. Sonographic appearance is similar to that of breast tissue with fibroglandular tissue interspersed between fat lobules. Doppler US shows mild internal vascularity.
MRI of the pelvis demonstrates a lobulated subcutaneous mass of the right vulva with no deep tissue invasion. Axial fat-suppressed T2-weighted MRI demonstrates a heterogenous mass with intermediate-to-high signal. Note the tiny intralesional T1 hyperintense foci indicating presence of fat.
DISCUSSION
The final diagnosis of this case is confirmed with US-guided core biopsy of the right vulvar mass with pathology showing benign breast tissue.
Ectopic breast tissue may develop anywhere along the milk line, which extends obliquely from the bilateral axillae, along the anterior abdominal walls, to the medial thigh regions. This condition occurs most frequently in the axillae.
Vulval ectopic breast tissue is rare and is often misdiagnosed. Similar to normal breast tissue, it can be affected by physiological changes under hormonal influence and various pathological conditions. It typically remains asymptomatic until enlargement occurs. Irrespective of the location, the appearance of ectopic breast tissue on imaging closely resembles that of normal breast tissue. On US, ectopic breast tissue appears as a heterogenous lesion of both fibroglandular and fatty tissues. On MRI, ectopic breast tissue appears as a subcutaneous mass with similar signal intensity and contrast enhancement to normal breast tissue.
This is a case of cyclosporin-induced proliferation of ectopic breast tissue involving the bilateral axillae and right vulva. Cyclosporin A has a potential trophic effect on cyclosporin A receptors in breast fibroblasts, which could explain the proliferation of multiple sites of ectopic breast tissue in our patient. Cyclosporin A-associated fibroadenomas have been described along with spontaneous regression of bilateral axillary accessory breast tissue after cyclosporin A dose reduction.
Ectopic breast should be considered as a possible differential for a subcutaneous mass occurring along the milk’s line, especially in renal transplant recipients.