Answer of July 2023
For completion of the online quiz, please visit the eHKAM LMS website.
Clinical History:
A 72 year-old man complains of increasing lower back pain after falling from a stool at home a few days ago, resulting in a back contusion. He is unable to walk (ambulatory premorbid status) and needs a wheelchair. Upon physical examination, there is bony tenderness at the thoracolumbar spine. Neurological examination of the limbs is normal.
Plain radiograph of the thoracolumbar junction (AP, Lateral)
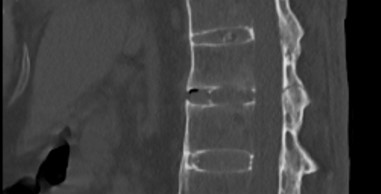

Plain CT (thoracolumbar junction; sagittal)
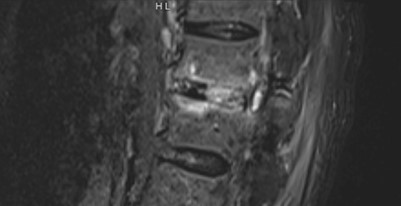
Plain MRI (T2/STIR; thoracolumbar junction; sagittal)
DIAGNOSIS
Ankylosing spondylitis with chalk stick fracture (three columns T12/L1 transdiscal fracture)
IMAGING FINDINGS
Plain film
Bamboo spine with ankylosed symdesmophytes, ossification of interspinatous ligaments (dragger spine) and ankylosed costovertebral joint, compatible with long-standing ankylosing spondylitis. Radiolucent fracture lines through T12 inferior vertebral body/ T12/L1 intervertebral disc space and posterior column are suggestive of chalkstick fracture.
Plain CT
Imaging features of bamboo & dragger spine and ankylosed facet joints. Acute three columns unstable T12/L1 transdiscal non-displaced fracture through bilateral pars interarticularis.
Plain MRI
Acute three columns unstable transdiscal non-displaced fracture through T12/L1 vertebra associated with bony edema. No associated epidural hematoma or cord contusion.
DISCUSSION
Ankylosing spondylitis (AS) is part of the rigid spine entity, within which also includes diffuse idiopathic skeletal hyperostosis (DISH), degenerative spondylosis (DS) and a surgically fused spine.
AS is an immune-mediated spondylosis. There is male predominance and is usually diagnosed in their 3rd decade of life. There is strong association with human leukocyte antigen (HLA)-B27 antigen. Its pathophysiology involves T cell-mediated attack on attachment sites of ligaments, tendons and joint capsules. The inflammation causes cartilage destruction and bone erosion, leading to reactive sclerosis and new bone formation.
AS is predominantly a clinical diagnosis. Yet diagnosis at early disease stage remains challenging. Vigilantly looking for imaging signs of AS helps pick up patients whose disease is yet undiagnosed. Sacroiliitis is the earliest sign, which is classically seen on anteroposterior radiographs as symmetric and bilateral subchondral erosions and sclerosis, followed by ankylosis at the inferior aspect of sacroiliac joints. Reactive sclerosis at anterior vertebral body erosions (also known as Romanus lesions) results in the “shiny corner sign”; further progression of Romanus lesions results in vertebral body squaring. Syndesmophytes cause ankylosis of vertebral bodies, creating a “bamboo spine” appearance. Ossification of the supraspinous and interspinous ligaments creates a long thin ossified line, resulting in the “dagger spine” appearance. Additional aspects that differentiate AS from other rigid spine entities include kyphotic deformity, ankylosis of the craniocervical junction and costovertebral joints.
The altered biomechanics and long lever arm of a rigid spine, alongside additional predisposition to osteoporosis in AS patients, make the spine prone to severe fractures even as a result of minor impact such as low-energy fall from standing or sitting. Other causes include transfer and intubation.
Hence, any patient with a rigid spine with acute back pain or trauma must be treated with a high suspicion for fracture until proven otherwise. While radiographs can aid diagnosis of AS, they are poor at depicting fractures. Both CT and MRI of the whole spine are recommended as first-line investigations, and that they should be used as complementary rather than alternative studies. This is due to the notoriously difficult diagnosis of fractures in rigid spines, as a result of transitional zone fracture locations, highly dystrophic or misshapen bone and body deformity. Radiologist’s role is to scrutinize for occult fractures, epidural hematoma or spinal cord injury; and to fully characterize the extent of injury to help guide management.
In rigid spines, fractures are often transverse. In AS particularly, the fracture is more commonly transdiscal. Nonetheless, they often extend to involve the vertebral bodies. Importantly, multiple noncontiguous fractures are not uncommon. At MRI, the fracture line has a hypointense signal, with the surrounding bone having low signal intensity on T1-weighted images and high signal intensity on T2-weighted images.
The historical Denis three-column concept helps classify spinal fractures morphologically. Fractures or ligamentous injury involving only one column are generally stable, while injuries with involvement of two or more columns are unstable. Nonetheless, the more comprehensive AO Spine classification system is now more preferred, as it incorporates fracture morphology, neurologic injury and has two modifiers (with M2 describing rigid spine entities, especially AS). It is important to recognize this M2 modifier as it can alter surgical management. For example, in thoracolumbar fractures, the fracture morphology is categorized into three types: (a) compression, with complete burst fractures being the highest subtype; (b) distraction, which are fractures that go beyond the vertebral body and cause ligamentous disruption; (c) translation, which is the most severe and involves displacement or dislocation of the spine.