Answer of May 2023
For completion of the online quiz, please visit the eHKAM LMS website or HKAM iCMECPD website.
Clinical History:
A 40-year-old patient with history of treated right parietal glioblastoma multiforme with adjuvant radiotherapy and stable disease for more than 5 years. He presented with headache, seizure and left hemiplegia. Symptoms resolved without specific treatment.
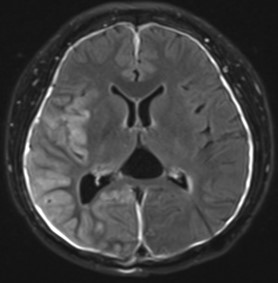
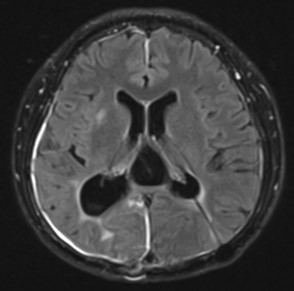
Fig. 1A Axial FLAIR post contrast fat suppression sequence at presentation
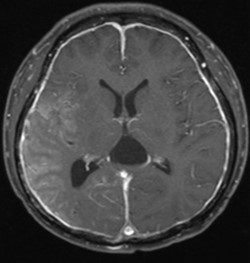
Fig. 1B Axial T1 post contrast fat suppression sequence at presentation
Fig. 2A Axial FLAIR post contrast fat suppression sequence on follow-up after symptoms subsided
Fig. 2B Axial T1 post contrast fat suppression sequence on follow-up after symptoms subsided
DIAGNOSIS
SMART syndrome
DISCUSSION
SMART syndrome is a rare, recurrent and late complication of irradiation with partial to complete recovery. It is more commonly seen in men and the clinical presentation includes migraine-like headache, stroke-like focal neurological deficit and seizure.
The pathophysiology is not well understood. The proposed mechanisms include cerebral hyper-excited status, resulting in impaired cerebral autoregulation and damage to the endothelium. Reversible radiation-induced vasculopathy may also contribute to the clinical and radiological presentation. However, no pathological correlation is identified on brain biopsy so far and histology cannot confirm the diagnosis. However, an open biopsy can be considered in order to exclude other differential diagnosis such as tumour recurrence.
Classical imaging findings include unilateral cortical gyriform swelling and enhancement with or without diffusion restriction, typically found at the parieto-temporo-occipital lobes.
Differential diagnosis of the combined clinical and radiological features would include tumour recurrence/leptomeningeal carcinomatosis, meningoencephalitis, reversible posterior leukoencephalopathy syndrome (PRES) or acute infarct. Diagnosis of SMART syndrome relies on exclusion of other differentials and demonstration of reversibility on follow up imaging. Therefore, clinical history plays an important role in reaching the diagnosis, in particular the clinical course and stability of background CNS neoplasm. Lumbar puncture shall be performed to exclude the possibility of CNS infection in appropriate clinical setting.
The clinical presentation and imaging features of acute infarct may simulate SMART syndrome. However, on imaging, SMART syndrome classically involves the grey matter with no/little white matter involvement and does not follow a particular vascular territory, as opposed to acute infarct. The cortical and unilateral involvement of SMART syndrome may also aid differentiation between PRES, which commonly shows bilateral and white matter involvement.
No consensus on the effective treatment of SMART syndrome has been established although anti-epileptics and steroid have been used in some of the reported cases.