Answer of July 2022
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 52 year-old women, was referred for a MRI right ankle because of chronic right ankle pain for several years. She did not have any trauma history. She has no other joint pain.
Fig 1a Sagittal fat-suppressed proton density-weighted image
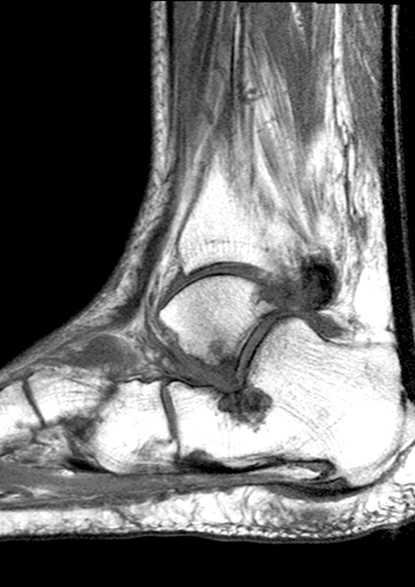
Fig 1b Sagittal T1-weighted image
Fig 2a Coronal fat-suppressed proton density-weighted image
Fig 2b Coronal T1-weighted image
Fig 3 Coronal T1-weighted image
Diagnosis:
Lateral hindfoot impingement with talocalcaneal impingement
Discussion:
Lateral hindfoot impingement is characteristically not related to an acute injury, but to chronic hindfoot valgus malalignment. This hindfoot malalignment is often due to posterior tibial tendon insufficiency, as this tendon is crucial in maintaining the longitudinal arch of the foot. The resulting hindfoot valgus malalignment is one of the components of acquired flatfoot deformity (pes planovalgus), and in severe cases a progressive lateral calcaneal subluxation occurs, such that the calcaneus may contact the fibula during weight-bearing.
Posterior tibial tendinopathy is a common cause of hindfoot valgus deformity. The prevalence of lateral hindfoot impingement has been found to increase with higher grades of posterior tibial tendon tear. Patients with posterior tibial tendon dysfunction experience both pain and disability. The pain is initially located along the medial aspect of the foot, often associated with swelling due to tenosynovitis. With progressive collapse of the longitudinal arch and development of a hindfoot valgus deformity, lateral foot pain develops, found to frequently relate to extra-articular talocalcaneal or calcaneofibular impingement.
Subluxation at the talocalcaneal joint has been shown to occur in symptomatic adults with acquired flat foot, involving a lateral translocation of the calcaneus into valgus malalignment, with the subluxation greater at the anterior and middle talocalcaneal articular facets than at the posterior facet, leading to reduction of articular contact surfaces at these joints. This subluxation causes a change in the overall shape of the foot, with flattening of the longitudinal arch, valgus of the hindfoot, and abduction of the forefoot. With a significant hindfoot valgus deformity, there will be a lateral shift of the main weightbearing forces at the ankle and hindfoot, from the talar dome towards the lateral talus and also to the fibula.
Regarding to MRI findings, subcortical bone marrow edema characteristically involves both opposing aspects of the talus, calcaneus, or fibula (Fig. 2a). The location of the bone marrow edema is characteristic, at the extra-articular region at the inferior apex of the lateral talar process and at the immediately subjacent aspect of the calcaneus at the apex of the angle of Gissane (Fig. 1a). The bony changes sometimes are seen to also involve the adjacent subcortical region of the anterosuperior calcaneal process, however if bone marrow edema is present all along the cortex around the margins of the sinus tarsi, this would not be characteristic and would instead suggest a diagnosis of sinus tarsi syndrome.
Peroneal tendon subluxation or dislocation has been reported in association with more severe cases of lateral hindfoot impingement, leading to tenosynovitis and tendinosis with possible longitudinal split tears or complete tendon tears.
Hindfoot valgus malalignment is a requisite for lateral hindfoot impingement to develop.
Recommended therapy for lateral hindfoot impingement usually involves surgery, due to the difficulty to stabilize a valgus deformity of the hindfoot with conservative measures such as medial wedge inlays or orthotics. At an earlier stage, physical therapy with Achilles tendon stretching may be warranted in cases of symptomatic flexible flatfoot. With a fixed deformity, or significant malalignment, surgery including calcaneal osteotomy is usually required and may provide hindfoot realignment without the restriction of movement of a fusion.



