Answer of April 2022
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 40-year-old man, chronic hepatitis B carrier, was admitted for right upper quadrant abdominal pain and fever. Laboratory test revealed mild leukocytosis (WCC up to 15 x 109/L) which subsequently normalized after starting intravenous augmentin. Liver, renal function tests remained normal. He underwent ultrasound, contrast CT abdomen during hospitalization. Tumour markers with AFP, CA 19.9 and CEA levels were normal. His abdominal pain and fever subsided with medical treatment and was fit for discharge afterwards. He underwent PET CT one week later.
Initial abdominal ultrasound (TS)
Ultrasound (LS)
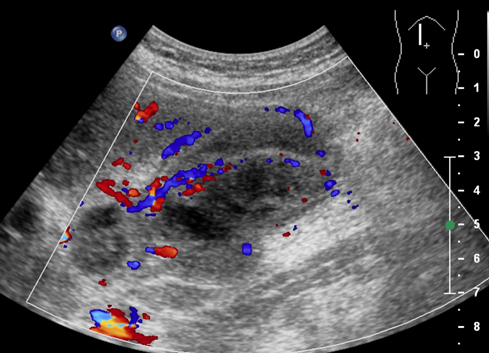
USG LS (with colour doppler)
Contrast CT abdomen (axial)
Contrast CT abdomen (sagittal)
PET CT fusion images (axial) 1 week after
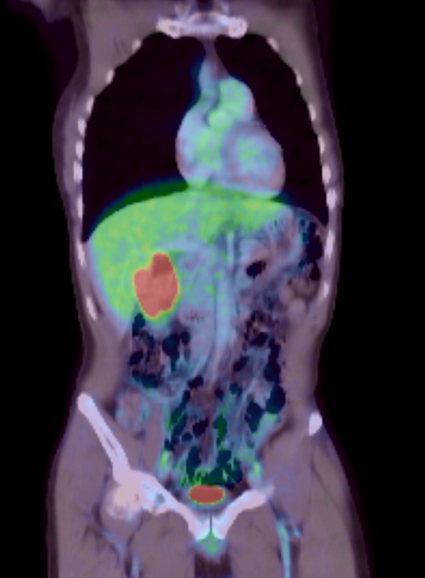
(PET CT fusion coronal)
DIAGNOSIS
Xanthogranulomatous cholecystitis (XGC).
DISCUSSION
Xanthogranulomatous cholecystitis (XGC) is a rare form of chronic cholecystitis, characterized by intramural deposition of lipid laden macrophage with background chronic active inflammation and fibrosis in histological exam.
It is postulated that intraabdominal pressure elevation of various etiology result in bile flow obstruction, leading to rupture of Rokinstanky-Aschoff sinuses with bile spillage, inciting inflammatory reactions.
Standard of management for XGC is cholecystectomy, which is both therapeutic and also enables definitive diagnosis with histopathological examination of gallbladder specimen through demonstration of aforementioned histological features. Immunohistochemistry with negative cytokeratin staining can help differentiation with gallbladder carcinoma.
Pre-operative diagnosis and differentiation with gallbladder carcinoma remain challenging due to overlapping clinical manifestations and imaging features. Both entities have peak incidence at around sixth to seventh decade of life with common association with choledocholithiasis. The clinical presentations of XGC are non-specific and may include abdominal pain, pyrexia, jaundice, palpable mass. Leukocytosis and tumour markers elevation can be present. Though a benign disease entity, XGC has been reported to be associated with coexisting gallbladder carcinoma in up to about 30% of cases.
Imaging features of XGC are characterized by diffuse (less commonly focal) gallbladder marked mural thickening. Presence of hypoechoic or hypoattenuating bands or nodules on ultrasound or CT is a characteristic finding, representing intra mural xanthogranulomata in chronic phase or abscess in acute phase. Continuous mucosal lining with mucosal hyperenhancement are also more favour XGC over gallbladder carcinoma, as XGC is a predominantly intramural process with while gallbladder carcinoma arises from the epithelium. Intraluminal polypoid mass formation have not been reported in cases of XGC and would more favour gallbladder carcinoma. Pericholecystic fat stranding or infiltration to liver parenchyma can occur in both XGC or gallbladder carcinoma, related to inflammatory process or tumour invasion, which also account for increased difficulty in cholecystectomy for XGC with surrounding inflammation and adhesion affecting local dissection.
FDG PET CT was not helpful in discriminating XGC from gallbladder carcinoma, as both conditions are associated with hypermetabolism. Studies have reported usefulness of chemical shift imaging in MRI to demonstrate intramural fat content favouring XGC, and lower incidence of restricted diffusion in XGC compared with gallbladder carcinoma.
For this patient, his age group was younger than that of gallbladder cancer. Diffuse marked mural thickening was present on ultrasound and CT, associated with hypermetabolism on PET CT. No discrete polypoid mass was noted. Regions of hypoechogenicity on ultrasound and hypoattenuation on CT represented intramural xanthogranuloma. The mucosal enhancement between these nodules are still preserved. No evidence of lymphadenopathy nor metastatic disease detected from PET CT. The overall features were more in favour of XGC. It was prudent to consider gallbladder carcinoma as a less likely differential. He underwent laparoscopic cholecystectomy which revealed dense adhesion in the Calot triangle and also fine pigmented gallstones. The final diagnosis of XGC was confirmed from histopathology. His post-operative recovery was uneventful.