Answer of March 2022
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 67-year-old female presented acutely with left loin pain and drop in blood haemoglobin level. Contrast CT performed showing subcapsular haematoma at the left kidney with contrast extravasation. Catheter angiogram was then performed.
On further questioning, she had a recent onset of fever, weight loss, diffuse myalgia, hypertension and progressive deranged renal function pending further investigations. The serum C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were also elevated.
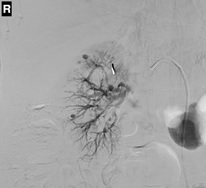
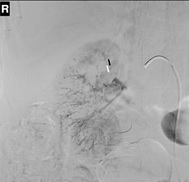
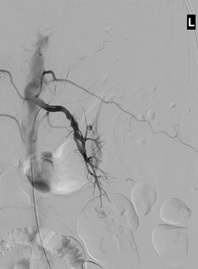
Selected images of right and left renal artery angiogram
IMAGING FINDINGS
Selected images of bilateral renal artery angiograms showed multiple microaneurysms involving the small branches of both renal arteries, mainly at the interlobular and arcuate branches. There were also multiple irregular stenoses involving the main trunk, segmental and interlobular branches of both renal arteries.
There were two foci of active contrast extravasation at the lower pole of left kidney, likely due to rupture of pre-existing microaneurysms, causing left renal subcapsular hematoma and the clinical presentations.
A surgical clip was also seen at the right upper quadrant abdomen in keeping with prior cholecystectomy.
DIAGNOSIS
C. Polyarteritis nodosa
DISCUSSION
Polyarteritis nodosa (PAN) is a systemic necrotizing vasculitis which typically involve the medium-sized vessels. It occurs more in men and commonly in the 5th to 7th decades. Most cases of PAN are idiopathic, although it can be associated with hepatitis B virus and human immunodeficiency virus. Exact pathogenesis of PAN is still poorly understood.
Recognition of PAN can be a clinical challenge given its wide spectrum of organ involvement and clinically symptoms with various severity. Kidneys are the most involved organ and involved in 70-80% of cases. Gastrointestinal tract, peripheral nerves, and skin are involved in 50% of the cases. Skeletal muscles, mesentery and central nervous system can also be involved.
Early diagnosis and treatment of PAN are necessary to prevent serious organ damage. However, diagnosing PAN can be challenging. There are no specific serological tests for PAN. Detailed history, physical examination, laboratory testing and radiological imaging are essential to establish the diagnosis and to exclude other differential diagnoses. Biopsy remains the gold standard for reaching the diagnosis. However, the diagnostic success rate may not be satisfactory (20-35%). The American College of Rheumatology published the 1990 criteria for the classification of polyarteritis nodosa. Three of the 10 criteria must be present for the diagnosis of PAN. A positive angiogram with typical findings is one of the 10 criteria. The criteria are listed as below:
1. Weight loss > 4 kg
2. Livedo
reticularis
3. Testicular
pain or tenderness
4. Myalgias, weakness or leg tenderness
5. Mononeuropathy or polyneuropathy
6. Diastolic blood pressure >90 mmHg
7. Elevated blood urea nitrogen (BUN) or creatinine
8. Hepatitis B virus infection
9. Arteriographic abnormality
10. Biopsy of small or medium-sized artery containing polymorphonuclear neutrophils (PMN)
Arteriography and cross-sectional imaging can be used as alternatives to tissue biopsy for the diagnosis. The characteristic finding was the presence of multiple microaneurysms up to 1cm in diameter. In renal arteries, the distal interlobar arteries and the arcuate arteries are most commonly involved. Beside the presence of microaneurysms, patients with PAN can also have luminal irregularities, stenoses and occlusion of the medium- and small-sized vessels. These angiographic changes are more sensitive and easily to be seen at catheter arteriogram. However, computed tomography (CT) and magnetic resonance imaging (MRI) are less invasive and provide additional information of end-organ damage (e.g. infarction) and other features of vasculitis (e.g. arterial wall thickening).
In a small percentage of patients with PAN as in our case, aneurysmal rupture may be the first clinical evidence of the disease. Embolization therapy is often the treatment of choice to stop the aneurysmal bleeding. Successful transcatheter embolization has been reported with different embolic materials, including microcoils and N-butyl cyanoacrylate (NBCA) glue. In our case, superselective glue embolization was performed to the ruptured aneurysms. In some literatures, prophylactic embolization of large aneurysms is also advocated due to underlying risk of rupture.
Patients with PAN can be treated by systemic steroid with or without the addition of another immunosuppressant. Choice of treatment depends on the distribution of the involved organs and disease progression. The 5-year survival rate for untreated PAN is 13%, and becomes 80% in patients receiving treatment. The prognosis of PAN varies depending on the age and organs involved. The five-factor score (FFS) developed by the French Vasculitis Study Group provides a simple prognostic estimation. The FFS was revised in 2011 and only includes four factors: age > 65 years, cardiac symptoms, gastrointestinal involvement, and renal insufficiency. One point is added for the presence of each factor. The 5-year mortality rates for scores of 0, 1, and ≥2 are 9%, 21%, and 40% respectively.