Answer of September 2021
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 61-year-old man had a history of Kappa light chain myeloma with baseline PET-CT showing extensive osteolytic lesions involving the whole skeleton (predominantly ribs and pelvis). The disease went into remission with combined chemotherapy VTD (bortezomib, thalidomide, and dexamethasone) with stem cell transplantation. He was put on regular Pamidronate (Zometa) infusion. He presented with chin swelling for one month. On examination there was submental soft tissue swelling extending from floor of mouth, swollen buccal sulcus with pus discharging into sinus. Necrotic alveolar bone was seen exposed from teeth 32, 33, 34 and 35. Radiographs were taken and urgent CT was arranged.
IMAGING FINDINGS
Orthopantomogram (OPG) and Radiographs of Mandible:
Edentulous maxilla. Few empty sockets at left mandible. Areas of sclerosis at both mandibular bodies involving the alveolar margin, lamina dura, surrounding the inferior alveolar canal, with loss of corticomedullary differentiation, more on the left side. Area of bony destruction and cortical erosion at parasymphyseal region with submental soft tissue swelling are noted.
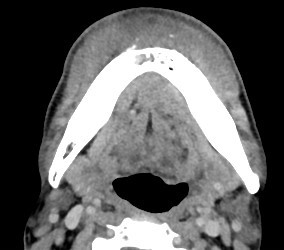
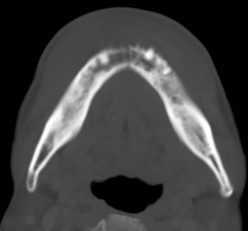
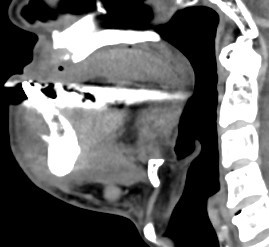
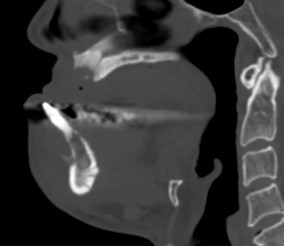
Contrast CT Mandible:
Areas of sclerosis seen at bilateral mandibular bodies surrounding inferior alveolar canal with loss of corticomedullary differentiation. Associated smooth periosteal reaction are seen. Lytic bone destruction is seen at parasymphyseal region with periosteal reaction. Soft tissue swelling at bilateral submental region and floor of mouth.
Overall features are compatible with osteonecrosis of jaw with submental infection.
DIAGNOSIS:
Bisphosphonate related osteonecrosis of jaw (BRONJ) complicated with submental infection.
DISCUSSION:
Osteonecrosis of the jaw (ONJ) is a consequence of prior radiation therapy (osteoradionecrosis; ORN) or certain antiresorptive medications. It is primarily a clinical diagnosis based on the presence of devitalized exposed bone. Although there is a need to exclude other disease processes such as neoplastic infiltration of bone and osteomyelitis, bone biopsy is generally avoided because it may cause damage and progression in ONJ. Therefore, radiology is playing an important role in confirming/ supporting the diagnosis, looking at the extent of disease and potential complications.
Bisphosphonates are one of the antiresorptive drugs that decrease bone turnover by inhibiting osteoclast-mediated bone resorption, are used to treat osteoporosis, Paget disease, pain from osseous metastases, and malignancy-related hypercalcemia.
Bisphosphonate-related osteonecrosis of the jaw (BRONJ) is defined by the American Society for Bone and Mineral Research as “an area of exposed bone in the maxillofacial region that has not healed within eight weeks after identification by a healthcare professional, in a patient who was receiving or had been exposed to a bisphosphonate and had not had radiation therapy to the craniofacial region”. BRONJ has been reported to manifest 6–60 months after initiation of treatment. The prevalence of ONJ is significantly high in those in patients receiving intravenous bisphosphonate treatment for cancer (1%-10%) than those received oral bisphosphonate for osteoporosis (variable between 0.0004% and greater than 0.04%). The underlying mechanism of BRONJ remains unclear.
Clinically it is a painful process and possible signs and symptoms include periodontal disease and non-healing mucosal ulcers, loose teeth and soft tissue infections.
Imaging appearances of osteoradionecrosis and medication-related osteonecrosis encompass a broad spectrum, ranging from lytic to mixed to sclerotic osseous changes. Other findings include sequestration, periosteal reaction and spreading of soft tissue inflammation.
Radiographic changes comprise of the following:
Osseous sclerosis (most common finding) varies from subtle thickening of the lamina dura and alveolar crest to attenuated osteopetrosis-like sclerosis. Sclerotic changes are often accompanied by periosteal bone formation, and this can be exuberant and cause anatomic expansion of the mandible.
Lytic changes appear as initially as areas of altered trabecular architecture and density, that progress to frank, patchy radiolucent bone destruction with cortical erosion and marked bone destruction. As the necrotic changes progress and coalesce, they isolate islands of necrotic bone sequestra.
Focal medullary sclerosis with disorganized microtrabeculae and poor corticomedullary differentiation in the suspected necrotic site has been described as a finding associated with early symptoms of tooth loosening or delayed socket healing after tooth extraction; this appearance may represent early imaging findings associated with BRONJ. Periosteal reaction and bony sequestrum may be predominant in advanced stages of the disease
CT in general shows a similar spectrum of findings of osteolysis and osteosclerosis but offers better extent delineation. Pathological fracture, bone sequestrum and associated soft tissue changes are better depicted.
Both CT and MRI are superior to clinical evaluation in evaluation of disease extent. MRI also evaluates both bone and soft-tissue involvement, which may be helpful in planning surgical debridement in intractable cases not responding to conservative treatment.
On MRI, variable signal intensity abnormalities on T1- and T2-weighted images possibly associated with the disease stage. ONJ is typically associated with decreased signal intensity on T1-weighted images; signal intensity changes on T2-weighted or short inversion time inversion-recovery (STIR) images and contrast-enhanced images show greater variability. The areas with increased signal intensity on T2-weighted or STIR images were thought to histologically resemble a chronic osteomyelitic pattern; areas with decreased signal intensity on T2-weighted or STIR images were histologically consistent with necrosis. Soft-tissue enhancement is variable and may involve the mylohyoid ridge, buccinator muscle, orbicular muscle, and masticator space. Cervical lymphadenopathy most commonly involves submandibular, followed by the submandibular angle and jugulodigastric chains
The top differential diagnosis is osteoradionecrosis, which has almost indistinguishable imaging features except that patients report a history of radiotherapy. Both BRONJ and malignancy have similar destructive appearances, often with periosteal bone formation. The periosteal new bone formation in BRONJ is regular, typically, paralleling the existing cortex. In contrast, periosteal bone formation in metastatic malignancies is more often disorganized with radiating spicules of new bone that are perpendicular to the existing cortex. Sclerosing osteomyelitis of Garré tends to affect young children and adults with asymmetric involvement of the mandible. The cortical layering of the bone (onion skinning) is typical. Osteosarcoma of the mandible typically presents with an osteoid matrix forming soft tissue mass with aggressive bone destruction.
Treatment is primarily conservative with maxillofacial/dental assessment, treatment of superimposed infection, bone necrosis, mitigating pain, maintaining dental hygiene. Surgery is generally to be avoided as it may aggravate the necrosis.
Our case received a course of intravenous antibiotic therapy (Amoxicillin-clavulanate and Metronidazole) resulting in resolution of submental infection. He underwent dental assessment and extraction of teeth 42, 41, 31, 32, 33, 34 and 45. Debridement of sockets, drainage of pus and removal of necrotic bone were also done with post-therapy OPG shown below. Pus culture yielded oral commensals. He continued chlorhexidine mouthwash for maintaining oral hygiene.