Answer of April 2021
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
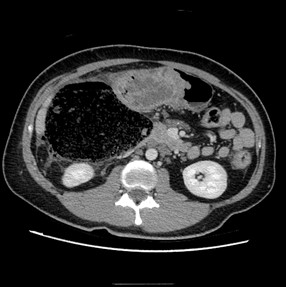
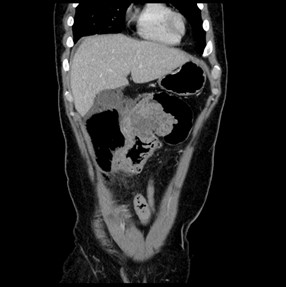
A 34 year-old presented to the emergency department with acute right lower quadrant pain, fever and tachycardia. Right abdominal peritoneal sign is positive on physical examination. Urgent computed tomography (CT) abdomen & pelvis with contrast was arranged because of unstable vital signs.
IMAGING FINDINGS:
Correct diagnosis is mucinous colonic carcinoma with rupture
DIAGNOSIS:
Mucinous colonic carcinoma
DISCUSSION:
Mucinous cancer is a distinct form of colorectal cancer found in 10–15% of patients with CRC. Mucinous cancer differs from non-mucinous adenocarcinoma in terms of clinical and histopathological characteristics.
It is less common in patients in Asian countries, and higher rates of mucinous cancer have been reported in Europe, North America and Australia. Furthermore, mucinous cancer is more commonly diagnosed in patients with inflammatory bowel diseases (IBD), such as Crohn's disease or ulcerative colitis, and in patients with a history of pelvic or abdominal radiotherapy,
Pathologically it is characterized by abundant extracellular mucous secretion comprising at least 50% of the tumor volume. Mucinous colonic tumors are more commonly associated with microsatellite instability with impaired DNA mismatch repair mechanisms.
Some imaging characteristics on computed tomography (CT) & magnetic resonance imaging (MRI) are discussed in the literature suggesting mucinous carcinoma over non-mucinous type. Mucinous colonic tumors tend more to occur at proximal colon. On CT, these included more severe and more eccentric bowel-wall thickening, heterogeneous contrast enhancement, more areas with hypoattenuation, and presence of intratumoral calcification. The solid portion of mucinous carcinoma showed less enhancement than that of non-mucinous carcinoma. On MRI T2-weighted images, mucinous colorectal carcinomas show high signal intensity due to the presence of abundant extracellular mucin. Unlike nonmucinous components with diffusion restriction, the mucin components of mucinous adenocarcinoma do not exhibit diffusion restriction
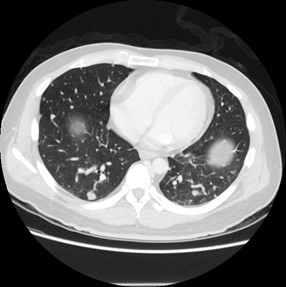
Mucinous colonic tumors are more commonly diagnosed at an advanced stage of disease, and more frequent with extrahepatic metastases (such as peritoneum or lung). They are known to have a propensity for higher incidence of lymph node metastasis, venous and lymphatic invasions, local recurrence, and distant metastasis. Furthermore, It has long been associated with an inferior response to treatment compared with conventional adenocarcinoma.
Therefore, it is of paramount importance for radiologists to distinguish between mucinous and nonmucinous colonic tumors on imaging.
Considering our case, the patient underwent urgent operation, confirming diagnosis of obstructing hepatic flexure colonic tumor with perforation and faecal peritonitis. Right hemicolectomy and ileocolic anastomosis was performed. He subsequently underwent molecular testing of the tumor including microsatellite stability, RAS and BRAF mutation status for a tailored option of oncological treatment. It was found to be microsatellite stable, with KRAS positivity. He is currently treated with Oxaloplatin, Xeloda with Bevacizumab.