Answer of January 2021
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
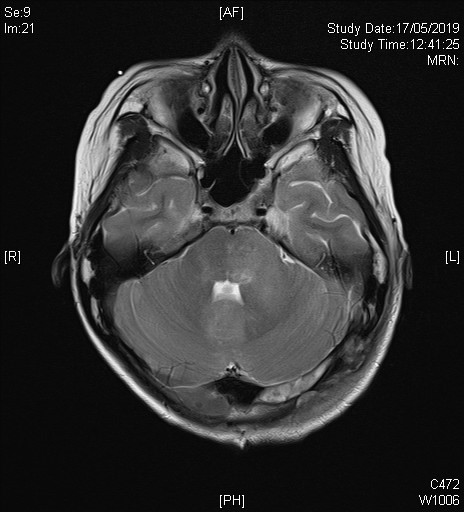
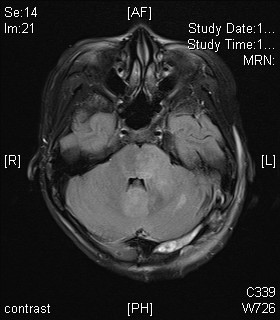
A 13 year-old girl with good past health presented with one-month history of increasing headache, associated with recent onset of vomiting and vertigo. She attended to emergency department and a plain Computer Tomography (CT) of the brain was performed urgently. Subsequent Magnetic Resonance Imaging (MRI) of the brain with contrast was performed.
 |
 |
 |
 |
 |
 |
 |
 |
Imaging Findings:
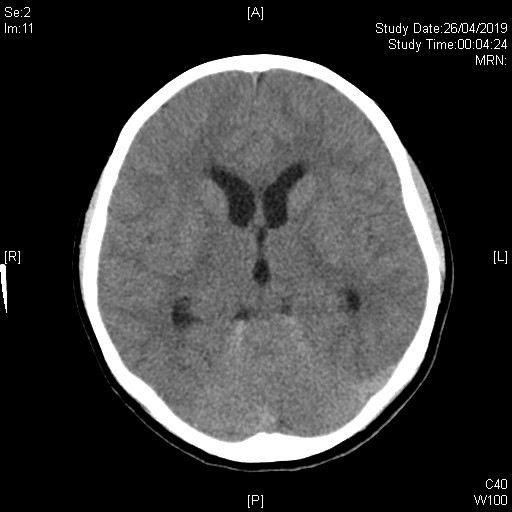
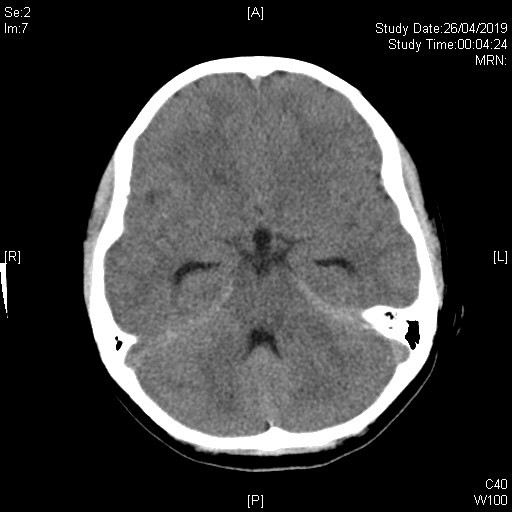
Initial plain CT brain shows an ill-defined lesion involving left cerebellar peduncle, left pons and cerebellar vermis. Associated mass effect onto 4th ventricle is noted. Dilatation of bilateral temporal horns of lateral ventricles and 3rd ventricle suggest early hydrocephalus.
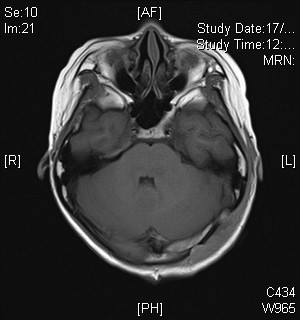
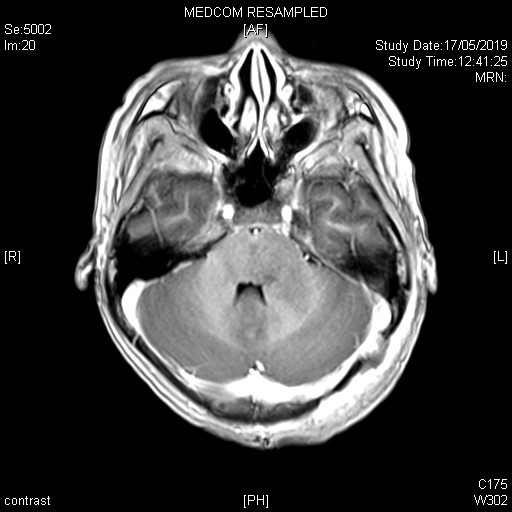
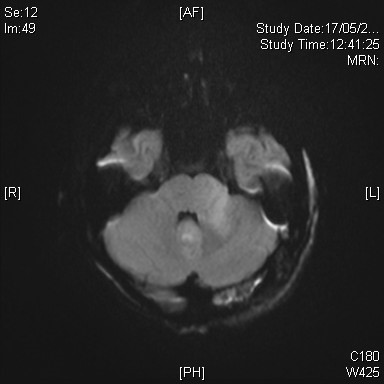
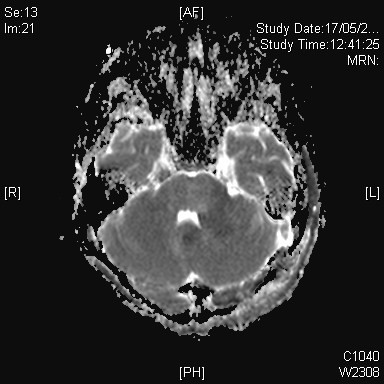
On subsequent MRI, there is an ill-defined mildly T2-weighted and FLAIR hyperintense signal lesion involving the left cerebellar peduncle, left pons, vermis, and bilateral cerebellar hemispheres. Corresponding restricted diffusion is noted. The previously noted hydrocephalus and associated transependymal oedema have resolved with ventricular drainage catheter inserted (not shown in selected image). Features favour the Wingless (WNT) subgroup of medulloblastoma in view of location and patient’s age.
Diagnosis:
WNT type Medulloblastoma
Discussion:
Medulloblastoma is the common malignant brain tumour of childhood, and is classified histologically as World Health Organization (WHO) grade IV tumor. It was thought to be a single entity but it was shown to be in four distinct molecular subgroups in the 2016 update of the WHO classification of CNS tumours. Four distinctive molecular subtypes are wingless (WNT), sonic hedgehog (SHH), group 3, and group 4, with distinct developmental origins, unique transcriptional profiles, diverse phenotypes, and varying clinical outcomes.
General imaging features on medulloblastoma on CT include a well-defined, solid, hyperdense lesion arising from vermis in the midline posterior fossa, in which it shows variable enhancement post-contrast. And on MRI it would generally appears iso- to hypointense compared to surrounding white matter on T1W images. Following intravenous gadolinium, it shows significant but variable and heterogeneous contrast enhancement. Due to the densely packed cellular components, it exhibits hypointense signal on T2W images with densely cellular components, and shows restricted diffusion.
WNT type medulloblastoma is the least common subtype of medulloblastoma (comprising about 10% of all medulloblastoma) and carries the best prognosis, with 5-year overall survival exceeding 90%. They are mostly sporadic and uniform in their genetic aberrations, histological pattern, and clinical presentation. The hallmark alteration in WNT tumors is the somatic activating mutations in exon 3 of β-catenin (CTNNB1), shown in 85% of WNT medulloblastoma and predictive of good outcome
They are equally distributed amongst boys and girls and commonly seen in older children and teenagers (peak incidence around 10-12 years old).
Radiogenomics or imaging genomics, which aims to define relationships between non-invasive imaging features (radio-phenotypes) and genomic data/ molecular markers (molecular phenotypes), plays significant role in identifying specific imaging features to these tumors. It had been suggested that tumor location was a key feature predictive of molecular subgroup. In one of the samples, WNT type medulloblastomas show a unique feature: cerebellar peduncle/cerebellopontine angle cistern localization (75%). The distinctive location predilection is not usually encountered in other molecular subgroups.
It was thought that these tumors arise from progenitor cells of the neural progenitors in the dorsal brainstem nuclei, therefore accounting for their midline location and close proximity to the dorsal brainstem.
Other characterising imaging features of WNT medulloblastomas include mostly isointense and homogeneous on T2W images. Peritumoral edema can be mild or absent. There maybe intratumoral hemorrhage or microcysts. Central nervous system metastatic disease is uncommon.
Surgical resection is the mainstay of treatment, which aims at histological proof, molecular subtyping and maximal tumour resection. Other adjuvant therapies include radiation therapy and chemotherapy.