Answer of November 2020
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 60-year-old woman with known history of hypertension, poorly controlled diabetes mellitus and hyperlipidaemia presented with one-week history of left sided involuntary movement. Urgent CT brain and MRI were performed.
|
Non-contrast CT brain |
|
|
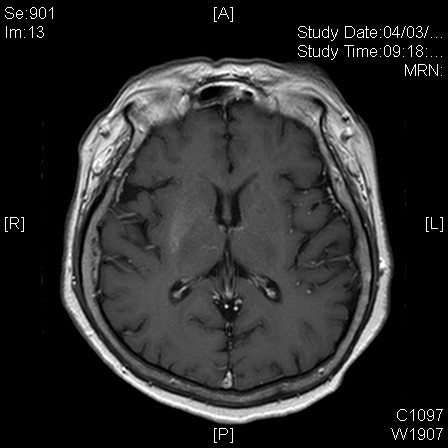
T1W |
T1W + contrast |
|
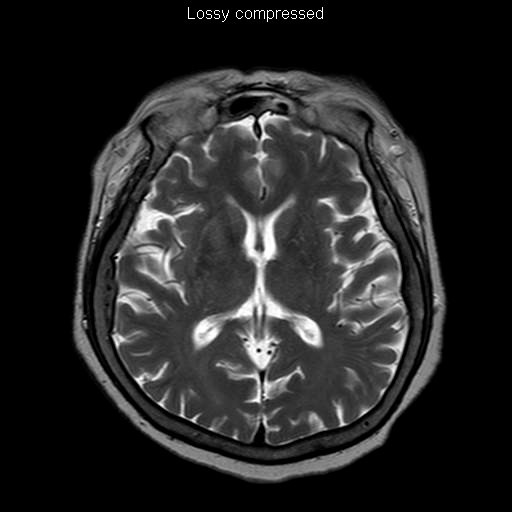
T2W |
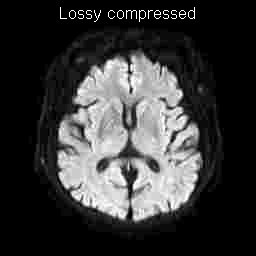
DWI |
|
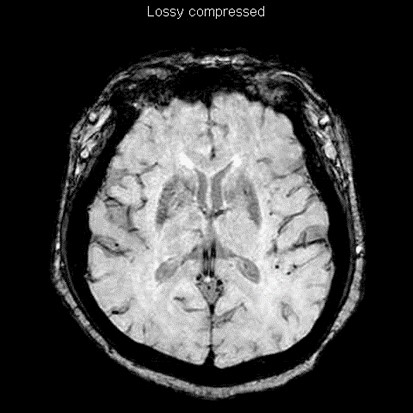
SWI |
|
Image Findings:
On non-contrast CT, there is hyperdensity at the right lentiform nucleus, which follows the contour of the basal ganglia, without mass effect or perilesional oedema.
On MRI, the lesion is hyperintense on T1-weighted images and isointense on T2-weighted images. There is no restricted diffusion on DWI and no blooming artefact on SWI. There is no contrast enhancement.
Diagnosis:
Non-ketotic hyperglycaemia hemichorea.
Discussion:
Non-ketotic hyperglycaemia hemichorea (NHH), also known as diabetic striatopathy, is a rare condition in poorly controlled diabetic patient presenting with hemichorea-hemiballismus syndrome, unilateral involuntary movement disorder. Bilateral movement disorder in non-ketotic hyperglycaemia is less common. This condition is particularly reported in elderly Asian patient with a female predominance.
In patient with NHH, CT brain would demonstrate hyperdensity of the basal ganglia contralateral to the side of hemichorea. The hyperdensity characteristically conforms to the shape of the basal ganglia, without mass effect or perilesional oedema, differentiating from hematoma and tumour.
MRI brain would confirm the basal ganglia abnormality, typically it is hyperintense on T1-weighted images, and there is no restricted diffusion. Imaging findings on T2-weight images can be variable. Differential diagnosis for hyperintense basal ganglia lesion on T1-weighted image includes metabolic disease such as hepatic encephalopathy and Wilson’s disease, striatocapsular infarction and hematoma. However, in most metabolic diseases, bilateral involvement in expected. NHH is unique entity commonly presents with unilateral involvement, contralateral to the side of clinical presentation. The putamen is most commonly involved. In most of the cases, the internal capsule is spared. The exact underlying pathophysiology producing such signal changes on imaging is still under debate.
In hemichorea-hemiballismus syndrome, the basal ganglia are usually being affected. Aetiologies include ischemic infarct, hematoma, tumour, and metabolic disease. Imaging is essential to differentiate the underlying cause and guide timely management.