Answer of July 2020
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
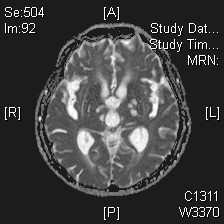
Clinical History:
A 68 year-old woman with good past health presented with drowsiness, vomiting and fall. Persistent drowsiness and drop in Glasgow-coma score (GCS) were noted. There was significant leukocytosis. Initial plain Computer Tomography (CT) of brain only showed small vessel disease and lacunar infarcts. Magnetic Resonance Imaging (MRI) was performed.
|
|
|
|
|
|
Imaging Findings:
Correct dianogsis is Cryptococcal meningoencephalitis.
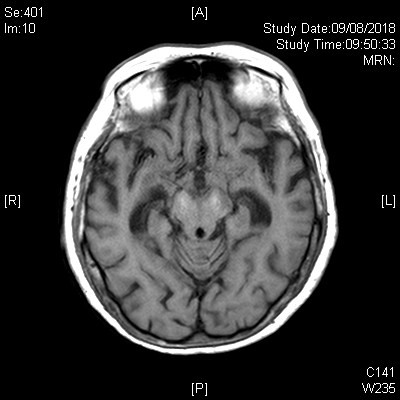
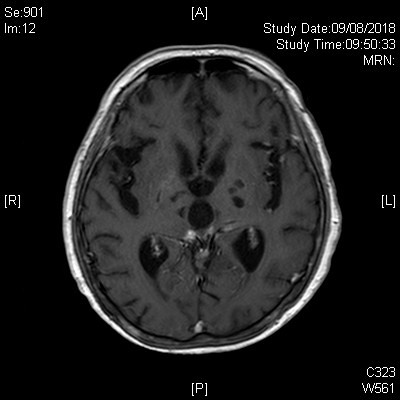
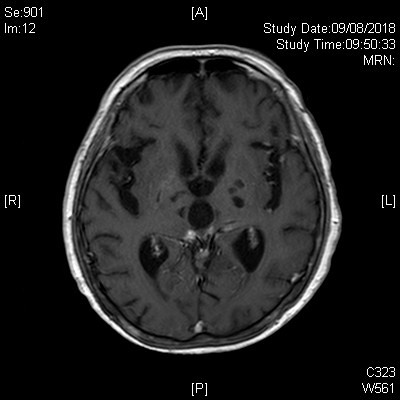
On given MR images, there is mild cerebral atrophy. Mild prominent ventricles especially temporal horns of bilateral lateral ventricles could indicate hydrocephalus. Multiple bilateral basal ganglia, thalamic non-enhancing T1W hypointense, T2W hyperintense lesions suggestive of gelatinous pseudocysts with dilated perivascular spaces. Nodular meningeal enhancement is noted in the basal cistern, interpeduncular cistern and along bilateral sylvian fissures, suggestive of basal meningitis. Overall features are compatible with Cryptococcal meningoencephalitis.
Mild bilateral lentiform nuclei and cerebral peduncle hyperintense T1 signals and small vessel ischemic changes are also noted within this study, the former could be due to metal (including possible Gadolinium) or calcium deposits.
Diagnosis:
Cryptococcal meningoencephalitis
Discussion:
Cryptococcus neoformans is the pathogen of Cryptoccus most commonly seen in nests and droppings of pigeons. Cryptococcus infection is mostly caused by C. neoformans (which accounts for 80%; mostly seen in central nervous system (CNS) infection) and the remaining 20% are caused by C. Gattii (more seen in the lung infection).
Cryptococcal infection is more commonly seen in immunocompromised patients, and C. neoformans is most common opportunistic CNS fungal pathogen in HIV-positive patients. Other predisposing factors include long term corticosteroids, advanced malignancy, organ transplant, diabetes insipidus.
Pathogenesis of cryptococcal meningoencephalitis was due to firstly inhalation of yeast cells into the lung. Together with defective host immune system in immunocompromised patient, the cryptococcal cells (which is small due to unilocular nature) proliferate and disseminate into CNS hematogenously crossing the blood-brain barrier causing meningoencephalitis. Parenchymal or subependymal invasion of cryptococci are mostly through perivascular and subarachnoid space. Budding yeast and mucoid material expand the perivascular spaces, producing gelatinous pseudocysts that are typically seen in the basal ganglia.
A range of MR imaging findings can be found in CNS cryptococcosis that can vary depending on the patient’s immune status. Classically there are clusters of dilated perivascular spaces found usually at the basal ganglia, which show hyperintense signal on T2-weighted and hypointense signal on T1-weighted sequences. They may show subtle peripheral enhancement. Coalescence of the dilated perivascular spaces results in formation of gelatinous pseudocysts. Other MRI features include leptomeningeal or pachymeningeal enhancement, presence of cryptococcomas, and ventriculitis. Cryptococcomas are defined as lesions in which cryptococcal organisms have involved parenchyma with granuloma consisting with lymphocytes, macrophages and foreign body giant cells. They show T1 hypointensity, T2/ FLAIR hyperintensity and variable enhancement. Menginitis or meningoencephalitis are leptomeningeal or dural thickening combined with focal parenchyma edema. Cerebral atrophy and hydrocephalus are more common presenting imaging findings, which are non-specific.
It should be noted that normal brain imaging findings are also seen (reported 47% by CT, 8% by MR) and therefore normal CT or MRI do not exclude the diagnosis.
Potential complications include hydrocephalus (most common), stroke, intracranial hypertension, and calcification.
Differential diagnosis includes other opportunistic infections such as tuberculosis and toxoplasmosis, as well as lymphoma.
Lumbar puncture was performed reviewed elevated protein, gram stain was negative in the cerebrospinal fluid (CSF). Subsequent investigation showed scanty growth of Cryptoccocus in CSF, decreased glucose, increased titre of anti-Cryptococcal antibody.
Patient was put on amphotericin B with fluconazole for treatment, but progress MRI revealed worsening meningoencephalitis changes. Improvement was noted after voriconazole. HIV testing was negative.
Treatment of CNS cryptococcosis involves the administration of antifungal agents such as amphotericin B and fluconazole.