Answer of June 2020
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 5-day-old full term neonate presented with bilious vomiting. Abdominal X-ray shows a large gastric bubble and paucity of distal bowel gas. An urgent water soluble contrast follow through was carried out, followed by a supplementary ultrasound study.
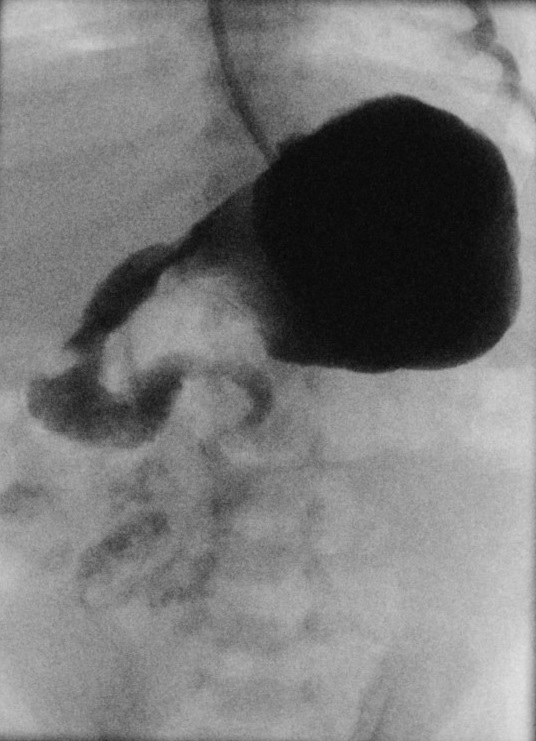
Water soluble contrast follow through:
Image 1 of 2
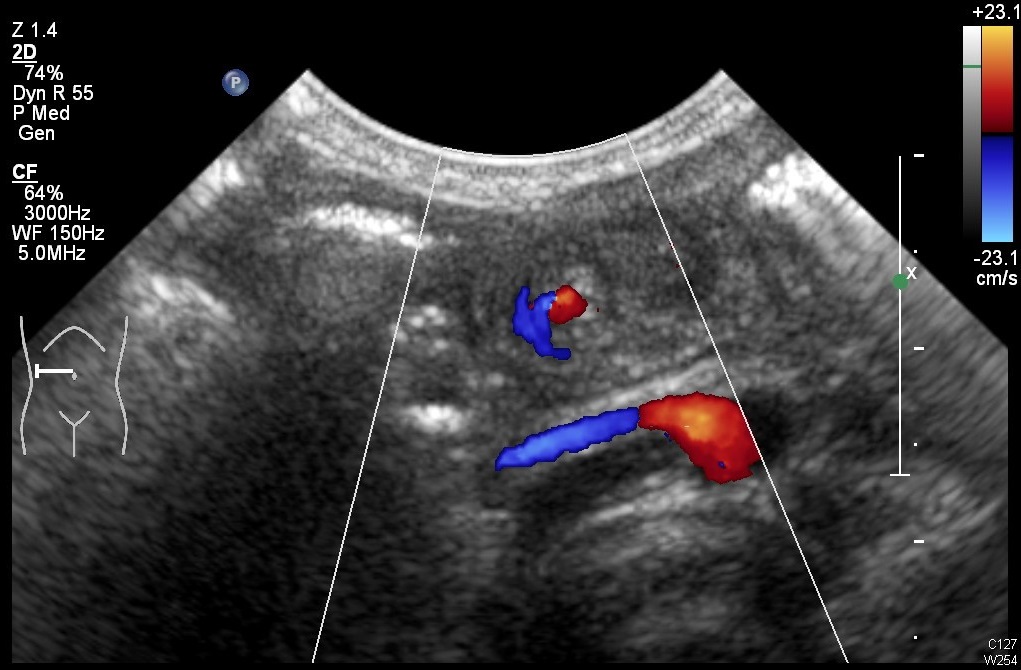
Supplementary abdominal ultrasound examination:
Image 2 of 2
Image Findings:
- Water soluble contrast follow through shows malpositioned duodenojejunal junction, which is located inferior to the duodenal bulb and does not cross the midline, suggestive of midgut malrotation. Corkscrew appearance of the distal duodenum and proximal jejunum is a sign of midgut volvulus.
- Whirlpool sign on abdominal ultrasound scan is feature of midgut volvulus.
Diagnosis:
Midgut volvulus can occur in any age, with more than 90% presents during the first three month of life. 60 - 80% of neonates with midgut volvulus present with bilious emesis, which is a surgical emergency. A delay in diagnosis can result in bowel ischaemia and eventual necrosis, peritonitis, shock and possibly death. Older children and adults may complain of non-specific symptoms such as chronic intermittent abdominal pain, non-bilious emesis and diarrhoea.
Midgut malrotation is the major predisposing factor for midgut volvulus. It is associated with other congenital abnormalities such as gastroschisis, omphalocele, diaphragmatic hernia, duodenal or jejunal atresia, and heterotaxy. Normally, the duodenojejunal junction (DJJ), also referred to as Ligament of Treitz, is positioned in the left upper quadrant of abdomen and the caecum is positioned in the right lower quadrant, resulting in a long fixed base that keeps the small bowel mesentery from twisting. Abnormal position of the bowel and fixation of the small bowel mesentery leads to shortening of the mesenteric root. The small bowel is prone to twisting around its mesentery, causing midgut volvulus. Malrotation is also associated with abnormal positional relationship of superior mesenteric vessels. The superior mesenteric vein is located to the left of superior mesenteric artery in midgut malrotation, which is opposite to its usual orientation.
Abdominal X-ray is usually the first imaging which is done in emergency setting. It may show features of intestinal obstruction.
Fluoroscopic upper gastrointestinal and small bowel follow through examinations are traditionally used to demonstrate the abnormal position of the DJJ. The DJJ is normally located retroperitoneally and to the left of the left L1 pedicle at the level of duodenal bulb. In malrotation, the DJJ is displaced inferiorly and to the right to the left L1 pedicle. The caecum may lie high and more to the left side. In the presence of a midgut volvulus, the twisted duodenum and jejunum gives a characteristic corkscrew-like appearance on fluoroscopic images, spiralling around the mesenteric vessels.
In midgut volvulus, whirlpool sign can be seen on ultrasound study due to whirling of mesenteric vessels. The abnormal positional relationship can also be demonstrated on ultrasonography and colour doppler studies.
It is more likely to encountered midgut malrotation and volvulus on computed tomography (CT) imaging in older children and adults. Swirling of bowel and mesenteric vessels at the site of the volvulus may be seen.
When a neonate presents with bilious emesis is diagnosed with midgut volvulus, urgent surgical repair is required to prevent bowel ischaemia and necrosis. The Ladd procedure is performed to alleviate intestinal malrotation. The Ladd’s bands are divided, and the mesenteric pedicle are widened. Appendix is also resected. The small bowel will stay at the right side of the abdomen, and the colon will remain on the left side after the operation.