Answer of April 2020
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
This 9-year-old boy presented to the Accident and Emergency Department for headache and vomiting for two months. On physical examination, papilledema was present.
 |
|
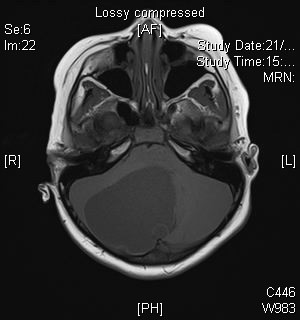
Fig1a (T1 weighted sequence of the brain) |
 |
|
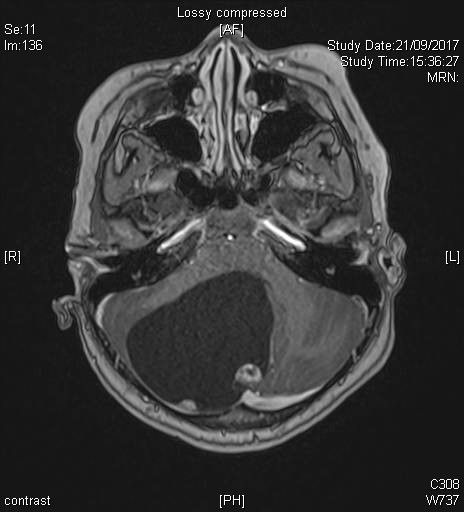
Fig1b (T1 post contrast sequence of the brain) |
 |
|
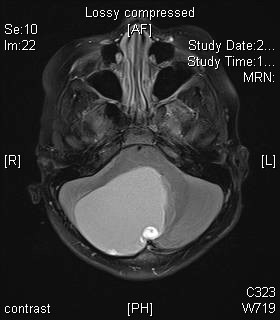
Fig1c (FLAIR sequence of the brain) |
 |
|
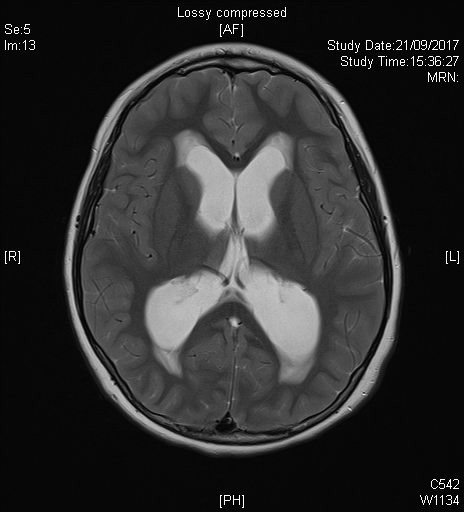
Fig1d (T2 weighted sequence of the brain) |
Image Findings:
Cystic lesion with enhancing mural nodule at the posterior fossa involving vermis and lateral hemispheres of the cerebellum, complicated with obstructive hydrocephalus as evidenced by dilatation of verntricular system above the 4th ventricular level and transependymal CSF flow.
Discussion:
Pilocytic astrocytomas are low grade astrocytomas that occur in young patients, with 75% occuring in first two decades of life, typically late in the first decade (9-10years), as in our case. They are considered WHO grade I tumors and has a relatively good prognosis. There is an association with NF1.
There are no clinical features that are unique to these tumours. Signs and symptoms are usually of several months' duration and are directly related to the size, location, and presence of associated hydrocephalus.
These tumors have a range of imaging appearances. On CT and MRI the tumor is typically a cerebellar vermian or hemispheric tumor which is cystic with enhancing mural nodule. Solid component is hypointense to siodense on CT, hyperintense on T2- weighted FSE and hypointesne of T1 weighted sequences reflexting the hypocellular and loosely arranged tumoral architecture. Calcifications are seen in around one-fifth of cases. The solid component is highly vascular with a deficient blood-brain barrier and therefore enhances avidly and homogenously despite being a low grade tumor. Occasionally the pilocytic astrocytoma may present with diffuse nodular enhancement of the leptomeninges, indicating intracranial or intraspinal pial dissemination. This does not imply a higher-grade tumor and like the tumor primary, tends to grow slowly.
Management of this case includes MRI whole spine to exclude metastastic disease and urgent neurosurgical referral for surgical decompression and resection.
Haemangioblastoma also has imaging appearance of a cystic lesion with mural nodule, However, these lesions are usually seen in adults, with smaller mural nodule and prominent serpentine flow voids on MRI which are not seen in pilocytic astrocytoma.