Answer of January 2020
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
56-year-old male patient was admitted for abdominal pain and fever. Patient was an alcoholic and had history of poorly controlled DM. Laboratory findings showed elevated white cell count and inflammatory markers. Contrast CT Abdomen was performed as initial investigation. Later the patient developed confusion and contrast MRI of the brain was performed for assessment.
Image Findings:
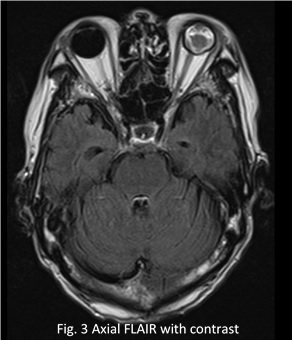
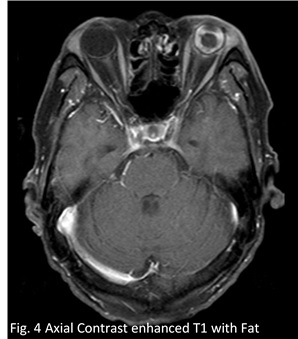
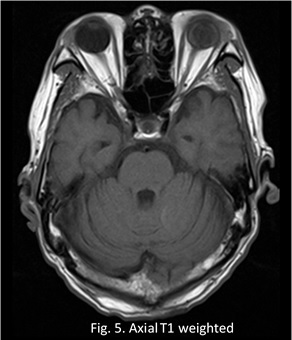
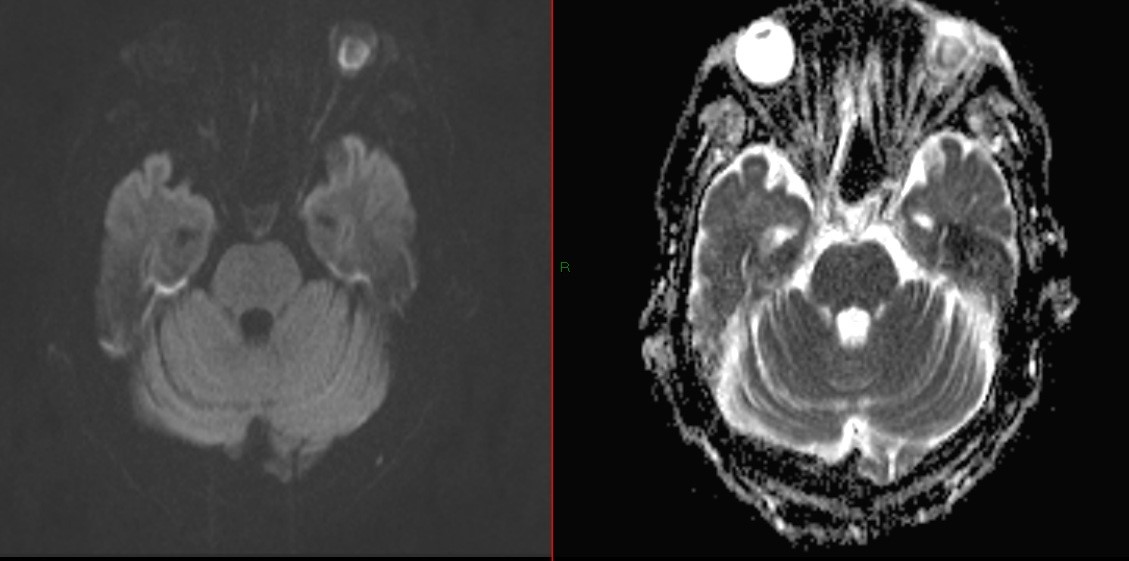
Diffuse scleral and uveal thickening with enhancement is noted in the left ocular globe. The signal of the vitreous on the left side is not completely suppressible on FLAIR sequence. The left eye is smaller with absence of lens, the result of prior phakectomy and vitreous sampling.
Diagnosis:
Left endophthalmitis, with history of prior phakectomy and vitreous sampling. The patient had disseminated sepsis, with blood culture yielding Klebsiella pneumoniae.
Discussion:
Endophthalmitis usually signifies infection, either bacterial or fungal, of the vitreous or aqueous humor. It is an uncommon ophthalmological emergency need to be treated early and aggressively in order to preserve visual function. Classical symptoms include red and painful eye with blurring of vision. Patient may have a history of recent eye surgery (e.g. cataract), penetrating trauma or partially/inadequately treated orbital cellulitis, as most endophthalmitis is secondary to exogeneous causes. On physical examination the affected eye shows conjunctival injection, chemosis, clouding of cornea, hypopyon, reduced/absent red reflex, poor fundal view due to intra-ocular inflammation and elevated intra-ocular pressure. There may be a reduction in visual acuity, which could deteriorate fast if untreated. Although it remains a clinical diagnosis, delayed and mis-diagnosis is not uncommon as classical symptoms may be lacking or not obvious. The most common mis-diagnosis is anterior uveitis. Usual causative organisms include Staphylococcus aureus, Klebsiella pneumoniae, Candida and Aspergillus species.
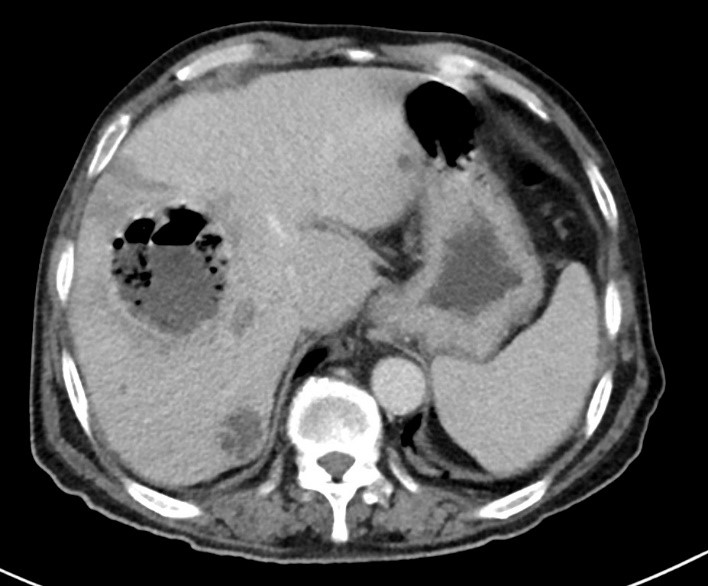
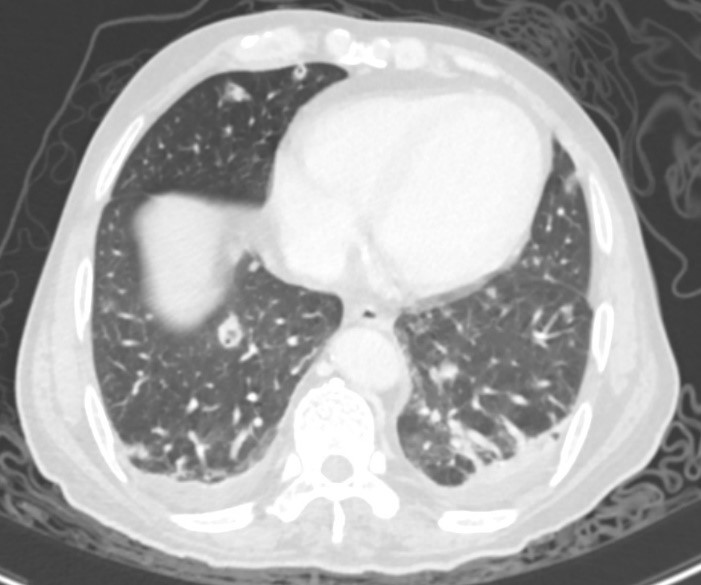
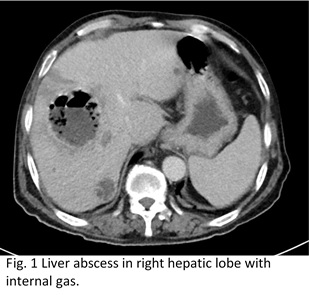
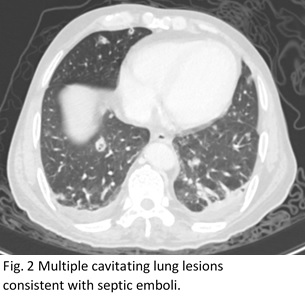
Uncommonly, endophthalmitis can develop secondary to hematogenous spread of pathogens (i.e. due to endogenous cause, accounting for 2-7% of all cases of endophthalmitis), e.g. bacterial septicemia, especially in patients who are immunocompromised (e.g. poorly controlled DM, renal failure) or intravenous drug addict. The patient in this case had concurrent liver abscesses and septic emboli within the lung (Fig. 1a and 1b), signifying the severity of disseminated Klebsiella infection.
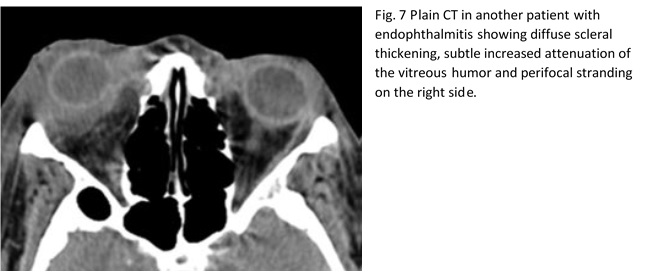
Changes of endophthalmitis on CT could be subtle, including proptosis, mildly increased attenuation of the vitreous and diffuse scleral thickening and adjacent stranding (Fig. 7, from reference 1). MRI is more sensitive to changes of endophthalmitis. The affected eye will show scleral and uveal thickening with enhancement and restricted diffusion. Due to proteinaceous exudate within the ocular globe, the vitreous humous will show reduced signal intensity on T2 weighted imaging together with non-suppressible signal on FLAIR sequence. Study1 has shown that diffusion weighted sequence is useful in following up patient with endophthalmitis. A decrease of restricted diffusion with increase in mead ADC value correlates with good treatment response, which may be otherwise difficult to be assessed clinically.