Answer of November 2019
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
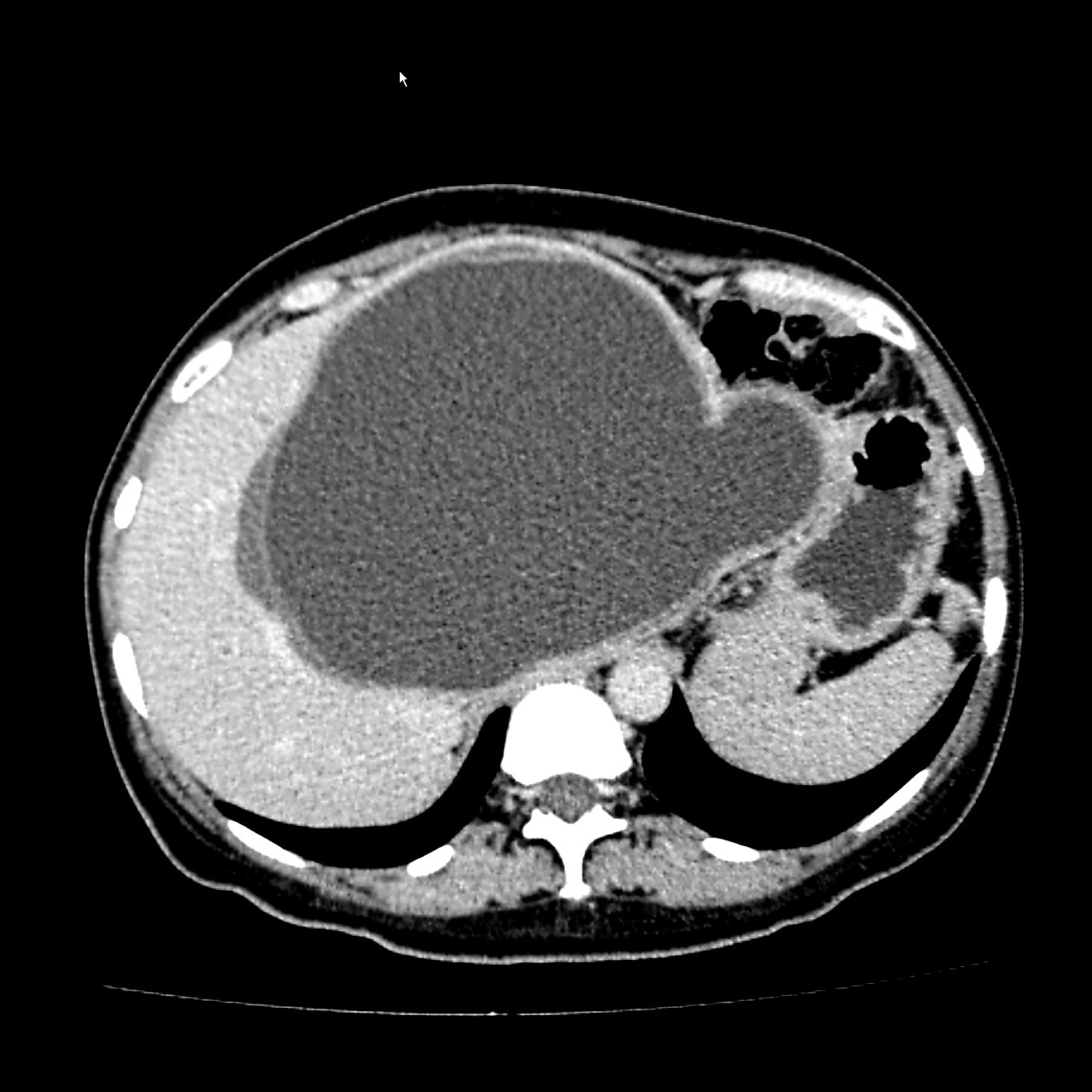
A 46-year-old lady complains of a right upper quadrant swelling for a year. She emigrated as a child from a farming community in Central Asia. Abdominal examination showed hepatomegaly.
 |
|
CT with contrast – coronal
|
 |
|
CT with contrast – axial
|
Discussion:
Echinococcosis is a parasitic disease caused by infection with tiny tapeworms of the genus Echinocococcus. Echinococcosis is classified as either cystic echinococcosis or alveolar echinococcosis.
Cystic echinocccosis (CE), also known as hydatid disease, is caused by infection with the larval stage of Echinococcus granulosus, a ~2-7 millimeter long tapeworm found in dogs (definitive host) and sheep, cattle, goats, and pigs (intermediate hosts). Although most infections in humans are asymptomatic, CE causes harmful, slowly enlarging cysts in the liver, lungs, and other organs that often grow unnoticed and neglected for years.
The life cycle of E granulosus involves two hosts. The definitive host is usually a dog. The adult worm of the parasite lives in the proximal small bowel of the definitive host, attached by hooklets to the mucosa. Eggs are released into the host's intestine and excreted in the faeces. Sheep are the most common intermediate hosts. They ingest the ovum while grazing on contaminated ground. The ovum loses its protective chitinous layer as it is digested in the duodenum. The released hexacanth embryo, passes through the intestinal wall into the portal circulation and develops into a cyst within the liver. When the definitive host eats the viscera of the intermediate host, the cycle is completed. Humans may become intermediate hosts through contact with a definitive host (usually a domesticated dog) or ingestion of contaminated water or vegetables. Once in the human liver, cysts grow to 1 cm during the first 6 months and 2–3 cm annually thereafter.
Hydatid disease primarily affects the liver and typically demonstrates characteristic imaging findings. However, there are many potential local complications (eg, intrahepatic complications, exophytic growth, transdiaphragmatic thoracic involvement, perforation into hollow viscera, peritoneal seeding, biliary communication, portal vein involvement, abdominal wall invasion). Furthermore, secondary involvement due to hematogenous dissemination may be seen in almost any anatomic location (eg, lung, kidney, spleen, bone, brain).
Diagnosis is usually made based on imaging features, although serological tests with indirect haemagglutination (IHA), immunoelectrophoresis (IEP) or Western blotting may play an adjunctive diagnostic role.
Cyst calcification usually occurs in the cyst wall, although internal calcification in the matrix may also be seen. US demonstrates a hyperechoic contour with a cone-shaped acoustic shadow. When the cyst wall is heavily calcified, only the anterior portion of the wall is visualized and appears as a thick arch with a posterior concavity. Partial calcification of the cyst does not always indicate the death of the parasite; nevertheless, densely calcified cysts may be assumed to be inactive.
CT is indicated in cases in which US fails due to patient-related difficulties (eg, obesity, excessive intestinal gas, abdominal wall deformities, previous surgery) or disease complications. CT has a high sensitivity and specificity for hepatic hydatid disease. Intravenous administration of contrast material is not necessary unless complications are suspected, especially infection and communication with the biliary tree.
CT may display the same findings as US. Cyst fluid usually demonstrates water attenuation (3–30 HU). Calcification of the cyst wall or internal septa is easily detected at CT. A hydatid cyst typically demonstrates a high-attenuation wall at unenhanced CT even without calcification. There is no clear explanation for this finding, which could be missed in patients with increased liver attenuation due to hemochromatosis, drugs (eg, amiodarone), and so on, or because of hepatic parenchymal enhancement following contrast material administration. Detachment of the laminated membrane from the pericyst can be visualized as linear areas of increased attenuation within the cyst. Daughter vesicles manifest as round structures located peripherally within the mother cyst. In our experience, they usually contain fluid with a lower attenuation than that of the fluid in the mother cyst.
Percutaneous aspiration is not recommended due to the risk of intraperitoneal seeding and severe allergic reaction. Chemotherapy with mebendazole and albendazole may be given to control disease but surgical resection offers the best chance of a complete cure in localized disease.