Answer of May 2019
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
This 55 year-old gentleman presented with unsteady gait for 6 months with mild left-sided weakness. CT brain and MRI were performed.
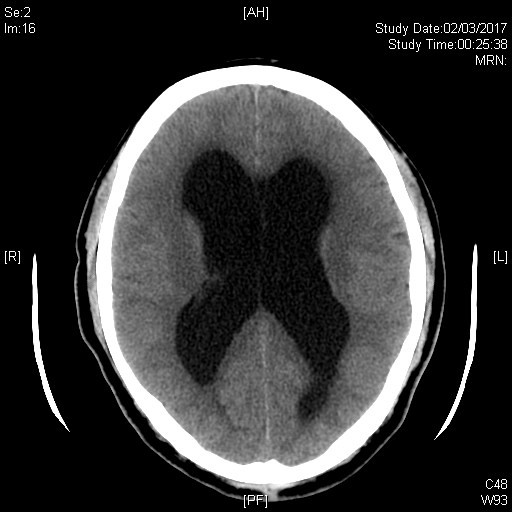
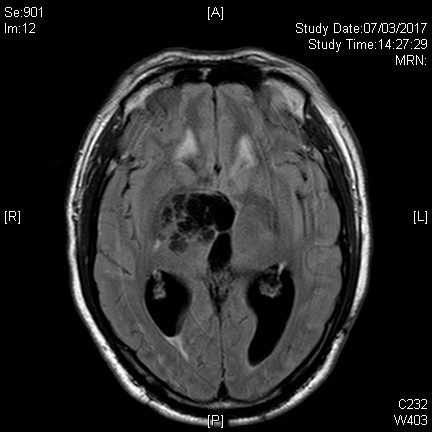
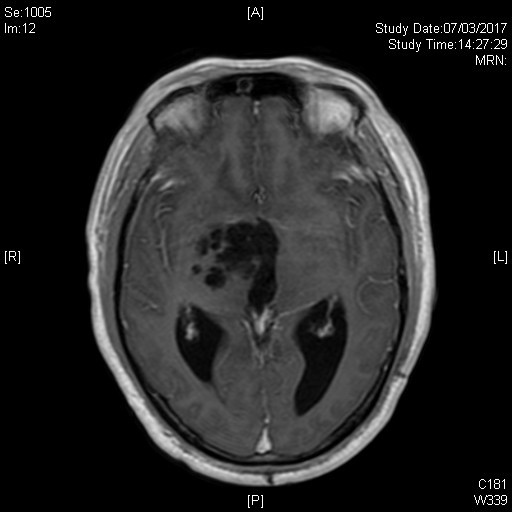
Image 1 of 10
CT
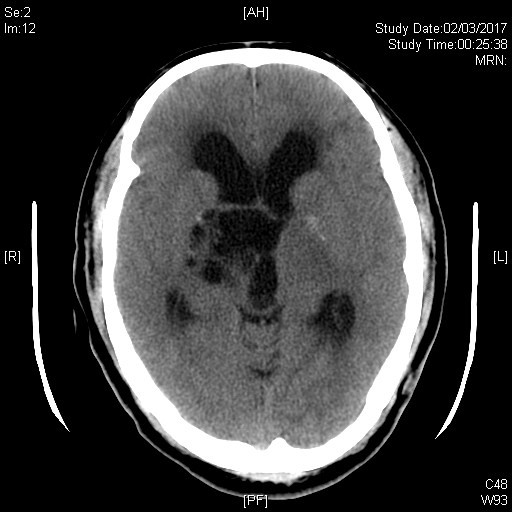
Image 2 of 10
CT
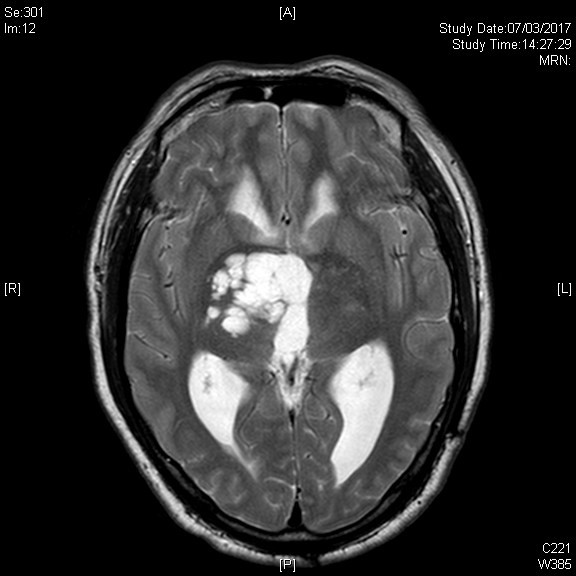
Image 3 of 10
T2 tse Ax
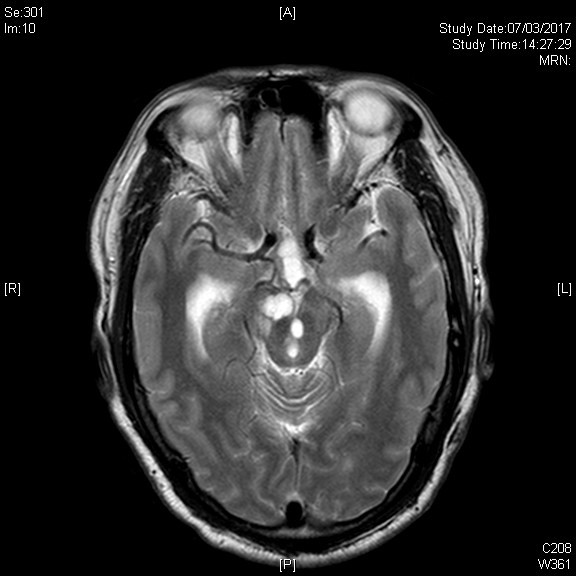
Image 4 of 10
T2 tse Ax
Image 5 of 10
T1 ffe Ax
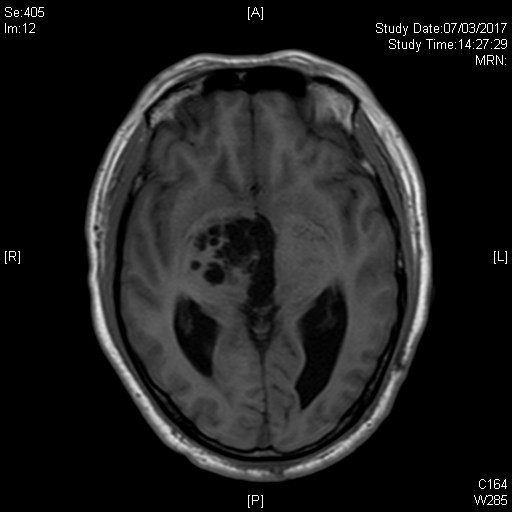
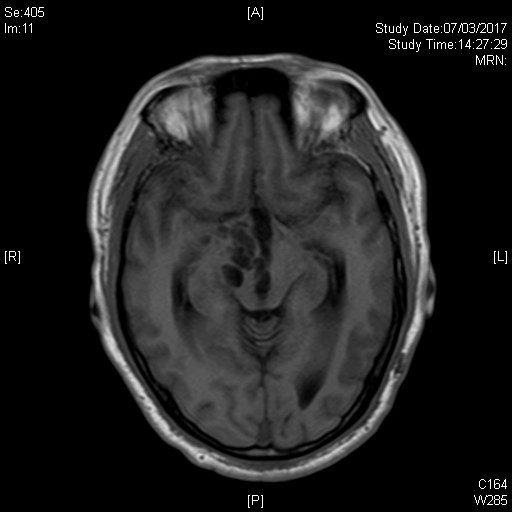
Image 6 of 10
T1 ffe Ax
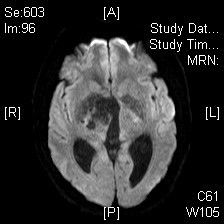
Image 7 of 10
DWI
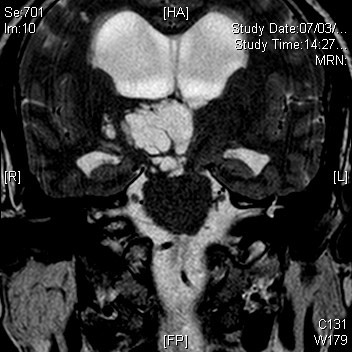
Image 8 of 10
T2 tse Cor
Image 9 of 10
T2 FLAIR Ax with gadolinium
Image 10 of 10
T1 ffe Ax with gadolinium
Imaging Findings:
- Multilocular non-enhancing cystic lesion in right thalamus, cerebral peduncle and midbrain
- Complete suppression of the cystic spaces on T2-weighted FLAIR sequence.
- No restricted diffusion on diffusion-weighted imaging.
- Mass effect indenting on third ventricle with hydrocephalus
- No abnormal perilesional signal intensities
Diagnosis:
Giant perivascular space
Discussion:
Dilated perivascular spaces (PVS) in the brain are interstitial fluid-filled structures lined by pia-mater that have accompanying patent penetrating arteries within, most commonly seen along the lenticulostriate arteries. They can be unilocular or multilocular and may have a radial pattern along the course of the penetrating arteries. PVS occur across all age groups and are more frequent and larger with advancing age. The cause of dilated PVS remains unknown though numerous theories have been postulated including increased permeability of arterial wall and obstruction/disturbance of interstitial fluid drainage/flow.
Rarely PVSs are markedly expanded and are termed giant PVSs. Some authors define giant PVS as larger than 1.5cm. Giant PVSs are most commonly located in mesencephalothalamic region. They are also seen in cerebral white matter and in the cerebellar dentate nuclei. They can exhibit mass effect and cause obstructive hydrocephalus when occurring in the mesencephalothalamic region as in our case. The signal intensities of typical PVS should follow cerebrospinal fluid in all sequences with no post-gadolinium enhancement. Complete suppression on FLAIR imaging is expected. There is no restricted diffusion on diffusion-weighted imaging as the compartments are communicating. Giant PVSs in cerebral white matter may have perilesional abnormal T2 and FLAIR hyperintensities as frequent as up to 50% of the time. It is postulated that the mass effect of the giant PVS causes chronic ischaemic change in adjacent white matter. Histopathological results typically show a pial-lined cyst with no evidence of neoplasm or infection.
Asymptomatic giant PVS can be managed by follow-up imaging for stability in size. Spontaneous regression of giant PVS without surgical intervention is rare. Giant PVSs with mass effect and obstructive hydrocephalus can be treated surgically with ventriculostomy, cyst fenestration, ventriculoperitoneal shunting or cystoperitoneal shunting. When the appearance is typical, surgical biopsy is unnecessary.