Answer of April 2019
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
This 16-year-old boy presented with knee pain after a knee “sprain”. No definite history of knee contusion is noted. No skin wound nor overlying skin change at the knee is noted. He is stable and afebrile at the time of examination.
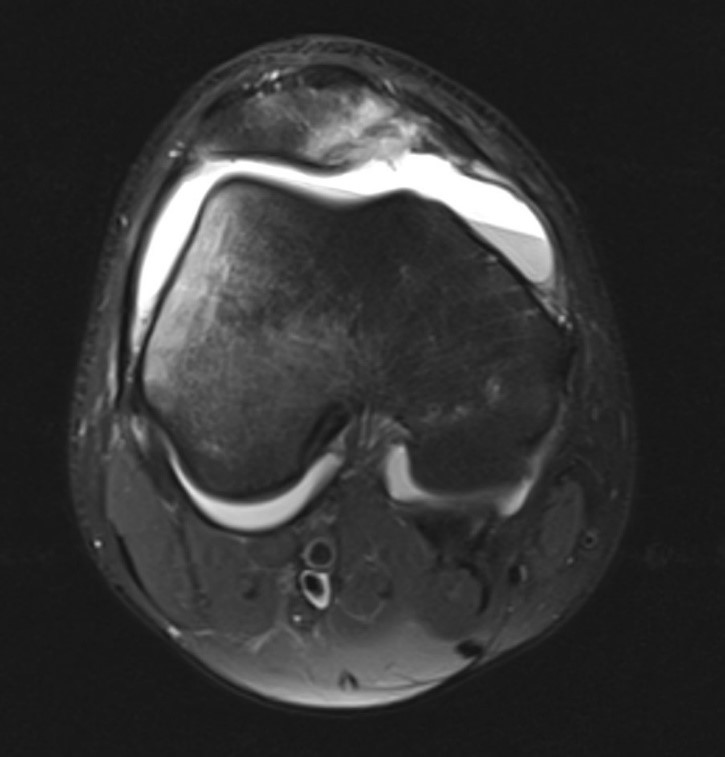
PD TSE FS TRA – Right Knee
Image 1 of 2
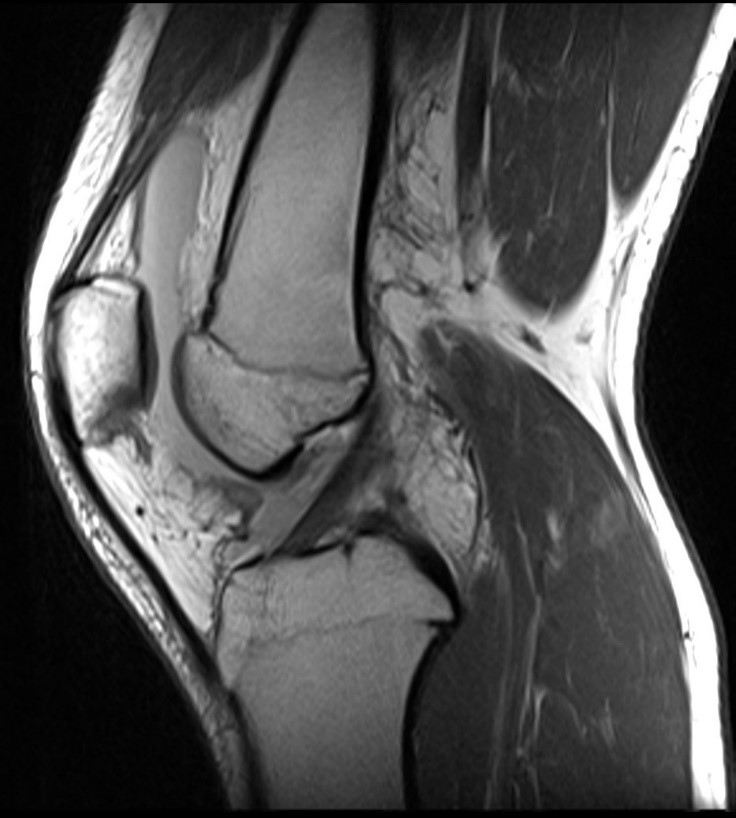
T1 TSE SAG – Right Knee
Image 2 of 2
Imaging Findings:
Abnormal knee effusion with dependent fluid-fluid level noted, suggestive of hemoarthrosis. Medial patellar facet and lateral femoral condyle edema is seen, suggestive of previous lateral patellar dislocation and kissing contusions.
Lateral patella tilting is seen. A shallow trochlea is noted. Suspected avulsion of the patellar attachment of the medial retinaculum is noted. Increased signal intensity is also seen at the medial patello-femoral ligament, suspicious of partial tear. The vastus medialis obliquus appears mildly displaced away from the adductor tubercle.
Patella alta is noted (Patella height ratio of 1.5 is noted). Tibial-tuberosity Trochleal-groove (TT-TG) distance by MRI = 1.3cm, which is within normal limits.
The lateral retinaculum shows wavy contour, suggestive of laxity
Diagnosis:
Lateral Patellar Dislocation of the Knee
Discussion:
First time patellar dislocation typically occurs in patients with twisting knee motions. The medial ligamentous stabilizers which then rupture, allowing the striking of the medial facet of the patella against the lateral femoral condyle. These causes the typical “kissing contusion” marrow edema.
Medial patellar soft tissue restraints include the medial patellofemoral ligament (MPFL), medial retinaculum and patellotibial ligament. The MPFL is believed to be the most important stabilizer in preventing lateral patellar dislocation.
The key to differentiate between MPFL and medial retinaculum on axial sequence is the presence of vastus medialis obliquus muscle underneath the MPFL, which is absent under the medial retinaculum.
Another associated features in lateral patellar dislocation may include a hemarthrosis, fracture of the patella and/or lateral femoral condyle, which were present in this case but the fracture fragments were not well demonstrated the selected images.
Predisposing factors of patellar instability can also be well delineated on MRI, which include trochlear dysplasia, high riding patella (patella alta) and lateralization of tibial tuberosity. The lateralization of tibial tuberosity can be quantitatively assessed on MRI by an abnormally increased TT-TG distance of more than 20mm on axial imaging.