Answer of September 2018
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
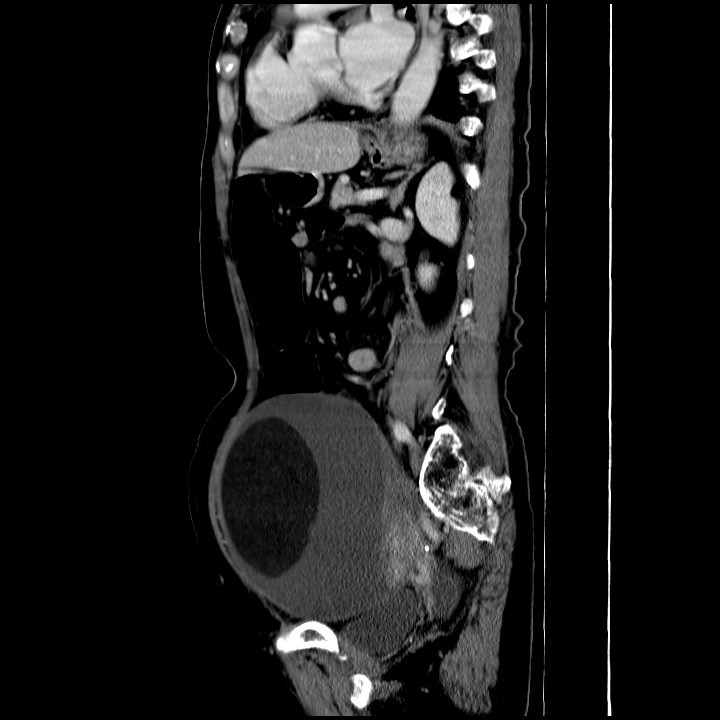
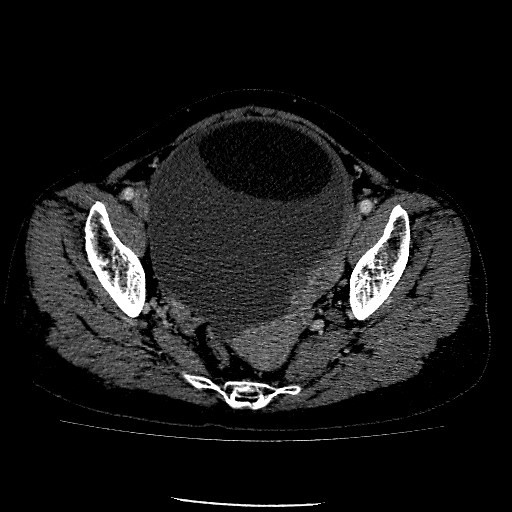
A 57 year old post-menopausal woman with vague abdominal discomfort for months presented to the Emergency Department with acute lower abdominal pain for 2 days associated with nausea and vomiting. Examination revealed a large tender pelvic mass ~20cm. Tumor marker CA 125 was elevated. Urgent contrast enhanced CT was performed.
 |
|
Image 1 of 3
|
 |
|
Image 2 of 3
|
 |
|
Image 3 of 3
|
Imaging Findings:
CECT abdomen and pelvis shows a large cystic adnexal mass with fat, fluid and enhancing soft tissue component. The enhancing soft tissue component shows border nodularity, and it forms an obtuse angle with the cyst wall. The ovarian mass is midline, with the uterus showing ipsilateral deviation towards the ovarian mass with ascites. These are features suggestive of torsion
Diagnosis:
Left ovarian mature cystic teratoma with torsion and malignant transformation into squamous cell carcinoma
Discussion:
Mature cystic teratomas are very common in women of childbearing age. They occur bilaterally in 10-17% of patients. They account for ~15% of all ovarian neoplasms, and tend to be identified in young women, typically around the age of 30 years.
Uncomplicated ovarian dermoid tend to be asymptomatic and are often discovered incidentally. They do, however, predispose to ovarian torsion, and may then present with acute pelvic pain. Imaging features of torsion on CT are somewhat non-specific. They include a midline pelvic mass rotated toward the contralateral side of the pelvis; deviation of the uterus to the side of the affected ovary; and ascites. Sometimes the whirled pedicle sign could also be seen on CT, though it is not always present.
Mature cystic teratomas are encapsulated tumours with mature tissue or organ components. They are composed of well-differentiated derivations from at least two of the three germ cell layers (i.e. ectoderm, mesoderm, and endoderm). Therefore components such as mature skin complete with hair follicles and sweat glands, sometimes luxuriant clumps of long hair, and often pockets of sebum, blood, fat, bone, nails, teeth, eyes, cartilage, and thyroid tissue are present.
Mature cystic teratomas with malignant transformation constitute 1% of all ovarian carcinomas. Malignant transformation is a known complication of mature cystic teratomas with a reported incidence of 0.17-2%. Differentiating benign and malignant ovarian tumors is very important as the surgery performed is much more extensive for malignant tumors. Intra-op frozen section remains the gold standard for such differentiation in mature cystic teratomas. However, some studies have reported up to 50% of cases reporting initial negative histological features of malignancy in squamous-cell carcinoma arising in a mature cystic teratoma, leading to inappropriate initial surgical treatments. Therefore, consideration for clinical, laboratory and imaging pre-operative predictors of malignancy have a role to play in surgical planning.
Malignant transformation is more common amongst patients older than 45 years with elevated tumor markers namely Ca-125, elevated CA 19.9, elevated SCC antigen. Imaging features on CT and MR that suggest malignant transformation would include the presence of soft tissue components with obtuse angle between the soft tissue components and the inner wall of the cyst; the nodular configuration of the inner border; the presence of enhancement, and large tumor size (>9.9cm).