Answer of June 2018
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
This patient was admitted for dizziness and left sided weakness. CT brain was obtained at admission. She had good neurological recovery and MRI brain was arranged at 3 months after discharge.
 |
|
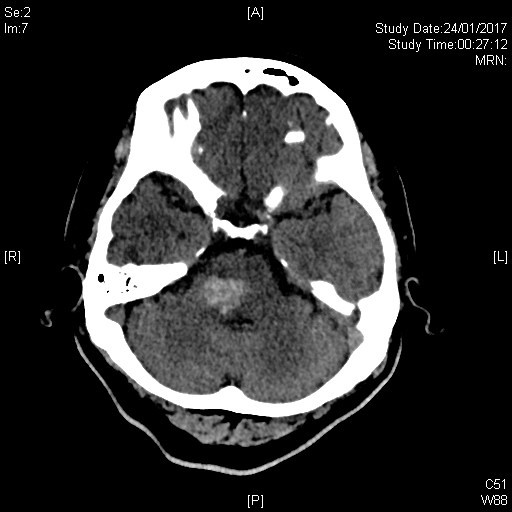
CT brain at admission |
 |
|
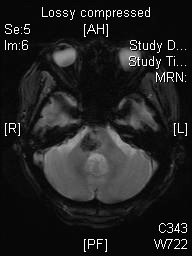
MRI brain 3 months after discharge |
 |
|
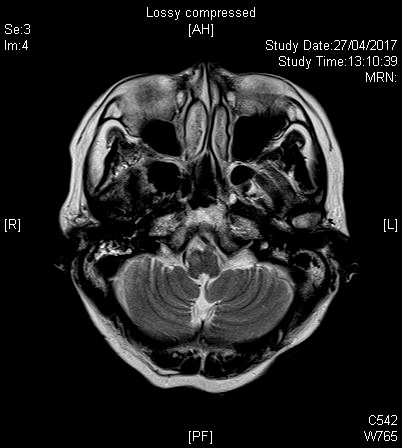
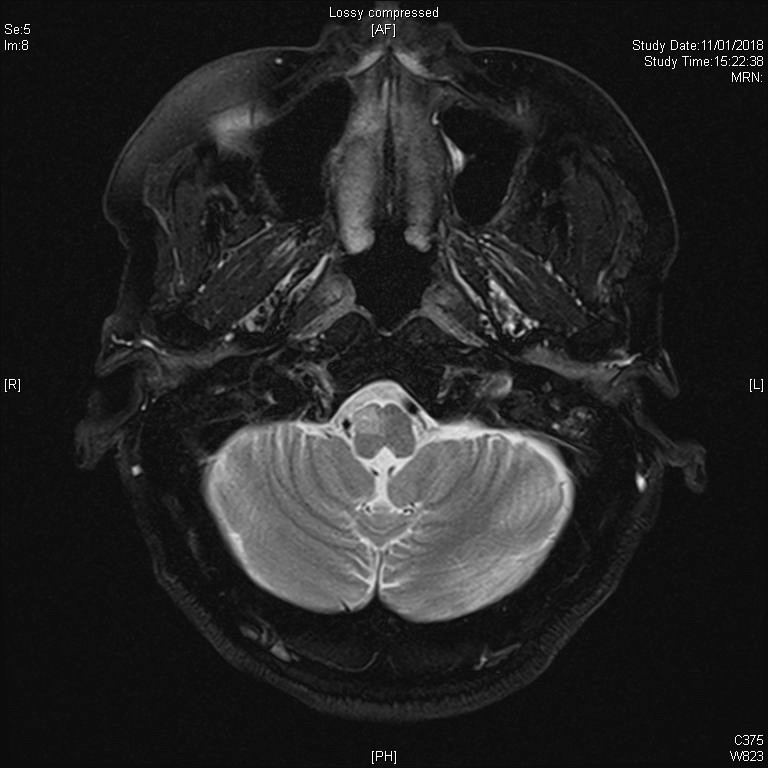
MRI brain 3 months after discharge |
 |
|
MRI brain 3 months after discharge |
 |
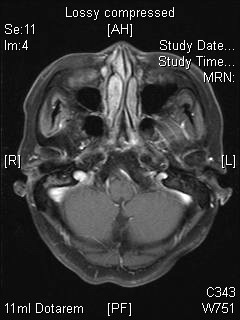
| Interval MRI brain after 9 months |
Imaging Findings:
1. CT brain at admission showed an acute hematoma at the right sided Pons.
2. MRI brain at 3 months after discharge showed an area of blooming artifact on susceptibility sequence, corresponding to site of prior right pontine hematoma. A focal T2w hyperintense lesion seen at the right sided medulla with no definite gadolinium enhancement.
3. Interval MRI brain 9 months afterwards showed interval enlargement of the focal T2w hyperintense lesion at the right sided medulla.
Diagnosis:
Hypertrophic Olivary Degeneration
Discussion:
Hypertrophic Olivary Degeneration (HOD) is a unique type of trans-synaptic neuronal degeneration. It is due to primary lesion (such as a hematoma in our case) in the Dento-Rubro-Olivary pathway (Triangle of Guillain-Mollaret). This pathway consists of ipsilateral inferior olivary nucleus (ION), ipsilateral red nucleus and contralateral dentate nucleus of cerebellum. Hence any lesion in ipsilateral central tegmental tract (connecting the ipsilateral red nucleus and inferior olivary nucleus), superior or inferior cerebellar peduncle which connects the contralateral cerebellar dentate nucleus can potentially cause this lesion.
Clinical features of HOD include palatal tremor or myoclonus in some patients, which usually occurs 10-11 months after primary lesion. Severe myoclonus may affect cervical muscles and diaphragm. A 2-5Hx, rest, postural and kinetic tremor of the upper limb might also be seen, also known as the dentatorubral tremor (Holmes Tremor).
Imaging features of HOD are best appreciated on MRI. CT most commonly shows evidence of primary injury, such as an acute hematoma in our case. However, the focal HOD is often not well appreciated. The best diagnostic clue of HOD on MRI would be a T2 hyperintense, non-enhancing enlargement of the ION. There are 3 distinct stages of HOD which could be well appreciated on T2w images. In lesions less than 6 months, there would be signal hyperintensity without hypertrophy of the ION. Both hyperintensity and hypertrophy of the ION are seen in lesions dated from 6 months to 3 years. In HOD more than 3 years, the hypertrophy resolves but hyperintensity persists. When the ION enlarges, the pre and post-olivary sulci are not as well seen compared to normal subjects.
Imaging differential diagnoses of HOD include those that cause a focal T2 hyperintensity at the brainstem, including demyelination, neoplasm (e.g. astrocytoma, lymphoma and metastases), infarct (PICA territory) and infection. Visualization of the primary insult, an expected time course of hypertrophy and a typical location (between the pre and post olivary sulci, instead of the lesion posterior to the post-olivary sulcus in PICA infarct) would help us in establishing the diagnosis of Hypertrophic Olivary Degeneration.