Answer of May 2018
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
- 5-year old male, term, normal birth weight
- Past medical history: Developmental delay, suspected neurofibromatosis 1 (multiple Café au lait macules)
- Admitted previously for febrile convulsion and right upper limb weakness. CT brain was unremarkable. He had good recovery.
- He presented again with convulsion, with left upper and lower limbs weakness and dysphasia. He then gradually recovered.
- MRI brain and digital subtraction angiogram were performed.
MRI Brain:
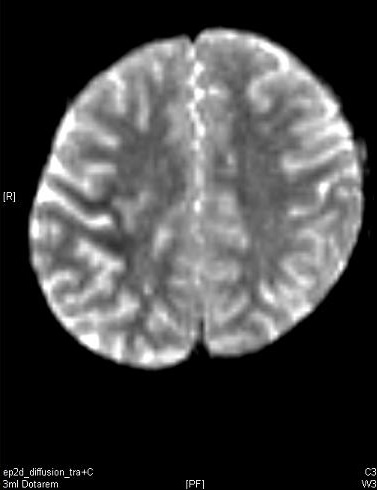
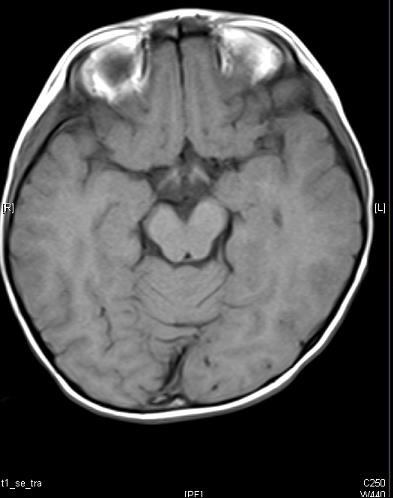
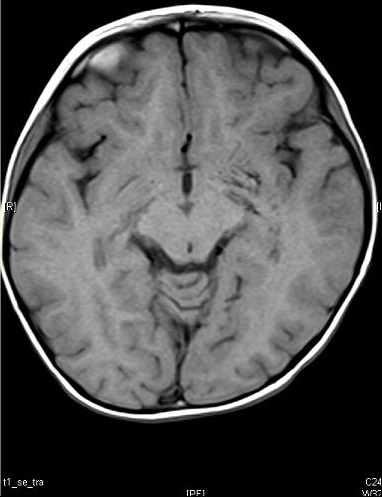
PD + T2 T1 Post-contrast
ADC DWI
T1W T1W
Diagnosis:
Moyamoya syndrome (associated with neurofibromatosis I)
Discussion:
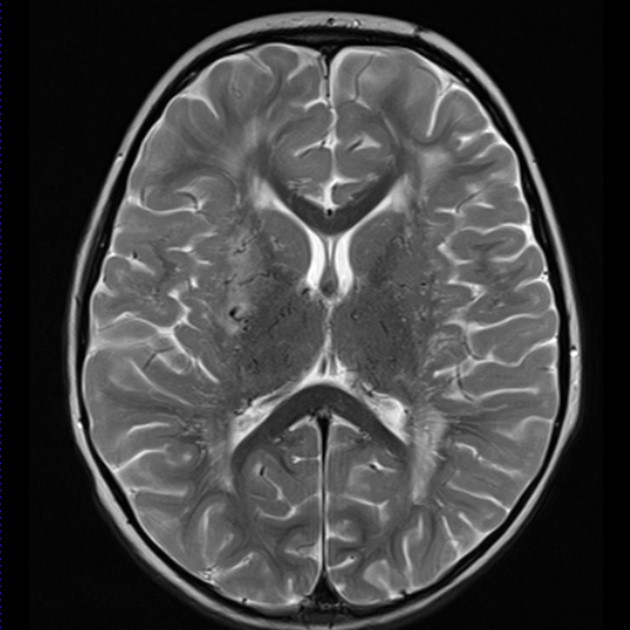
- MRI brain showed T2W hyperintense signal over right centrum semiovale, which was enhancing on post contrast images. It demonstrated restricted diffusion on DWI and ADC. These could represent acute / subacute infarct. T1W images showed reduced flow voids in the internal and middle cerebral arteries coupled with prominent flow related signal voids through the basal ganglia.
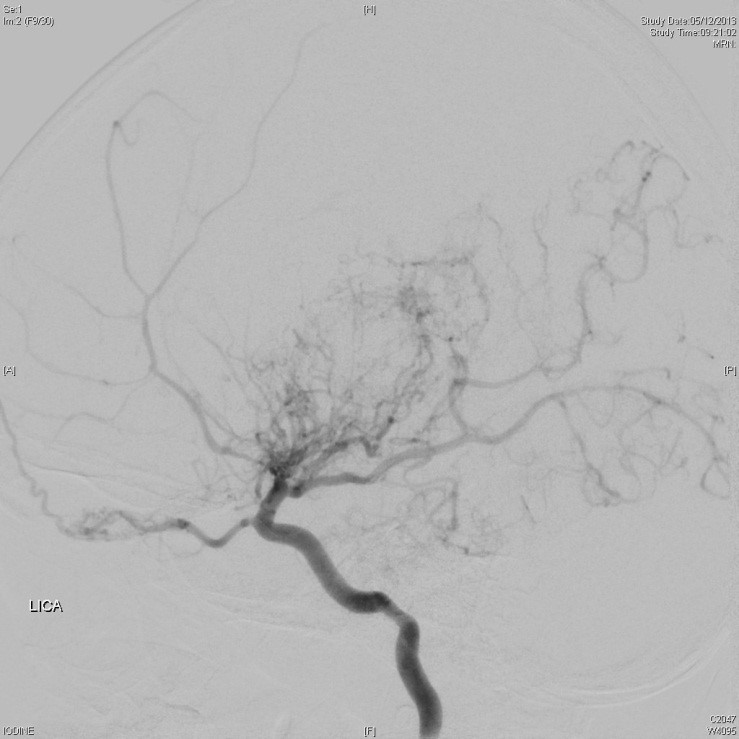
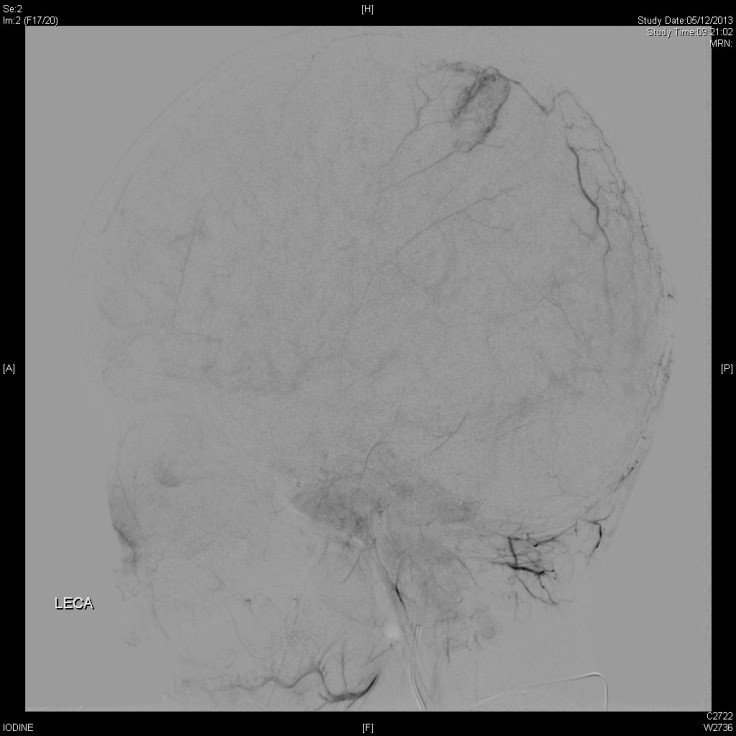
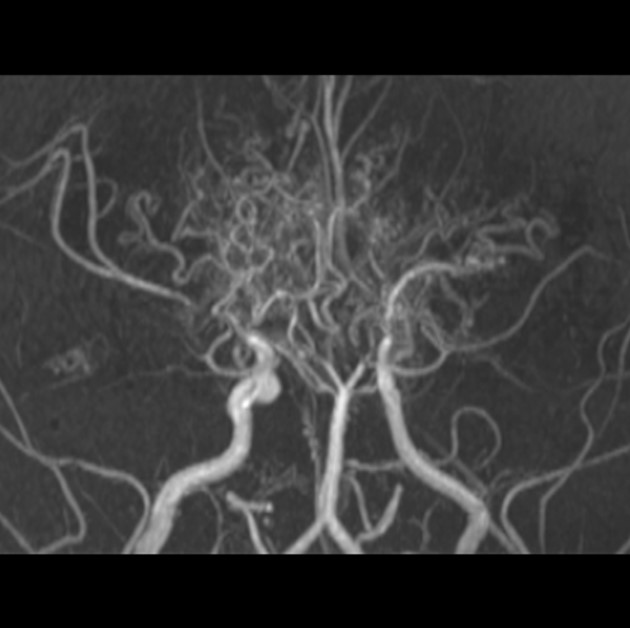
- Internal carotid and external carotid angiographic images (lateral projections) showed abrupt cut-off at bilateral terminal internal carotid artery(ICAs) and middle cerebral artery(MCAs) with collateral vessels at basal ganglia region. Collateral vessels are seen arising from occipital transosseous branches.
- Moyamoya syndrome refers to progressive stenosis of the intracranial internal carotid arteries and their proximal branches, with compensatory development of collateral vasculature (at the apex of the carotid, on the cortical surface, leptomeninges, and branches of the external carotid artery supplying the dura and the base of the skull.)
- Characteristic moyamoya vasculopathy occurring in presence of associated conditions is referred to as Moyamoya syndrome. These associated conditions include sickle cell disease, neurofibromatosis type 1, previous irradiation, an Down’s syndrome.
- If there is no known associated condition, the term moyamoya disease is used.
- Pathological findings show vessel occlusion resulting from a combination of hyperplasia of smooth-muscle cells and luminal thrombosis, which could lead to cerebral Ischemia. Moyamoya-associated collaterals are generally dilated perforating arteries, with combination of fragmented elastic lamina, thinned media in the vessel wall, and the presence of microaneurysms, which are prone to hemorrhage.
- The disease has bimodal recurrence, and incidence peaks are at 5 and 40 years old.
- Presentations include stroke, transient ischemic attack, cerebral hemorrhage, seizure, and headache.
- Characteristic CT findings include obliteration of the supraclinoid ICAs with numerous collaterals, cerebral / intraventricular hemorrhage. MRI can show reduced flow voids in ICAs, MCAs, coupled with prominent flow voids through the basal ganglia and thalamus from moyamoya-associated collateral vessels (puff of smoke).
Examples:
Surgical treatments make use of the external carotid artery as a source of new blood flow to the ischemic hemisphere, including direct: superficial temporal artery directly anastomosed to a MCA branch, and indirect: encephaloduroarteriosynangiosis, encephalomyoarteriosynangiosis and drilling of burr holes.