Answer of April 2018
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
An afebrile eleven-month-old boy presents with poor weight gain, abdominal mass and deranged liver function tests. The relevant chest/abdominal radiograph, ultrasound and contrast-enhanced CT scan of the abdomen were subsequently performed.
CHEST AND ABDOMINAL RADIOGRAPH
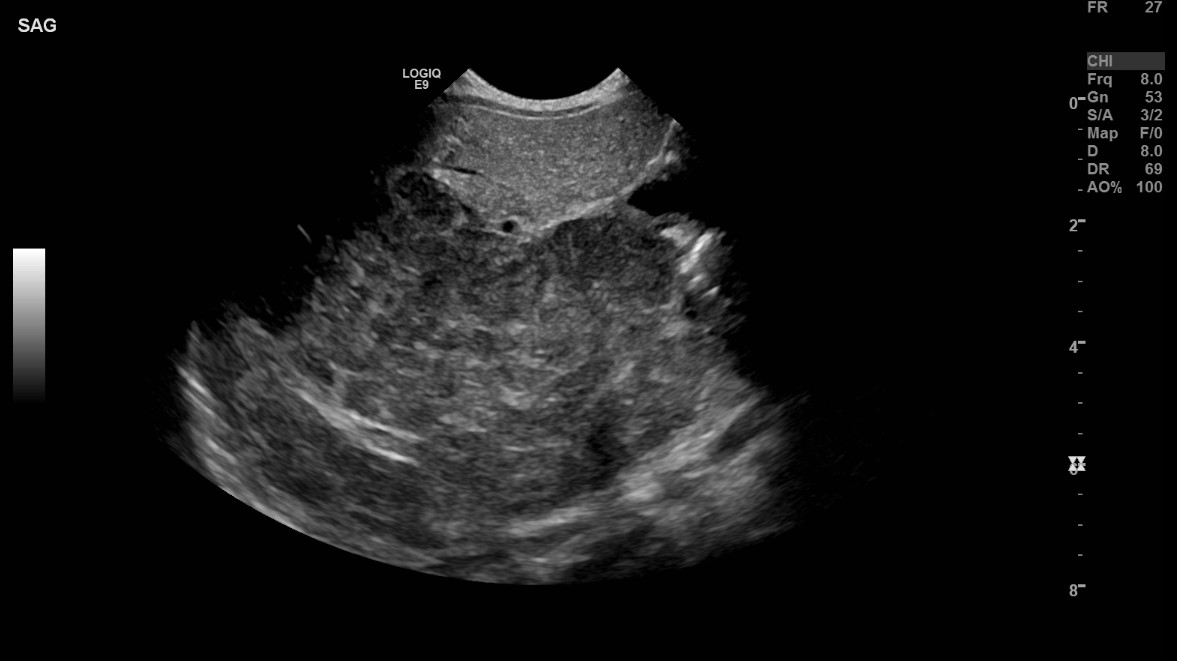
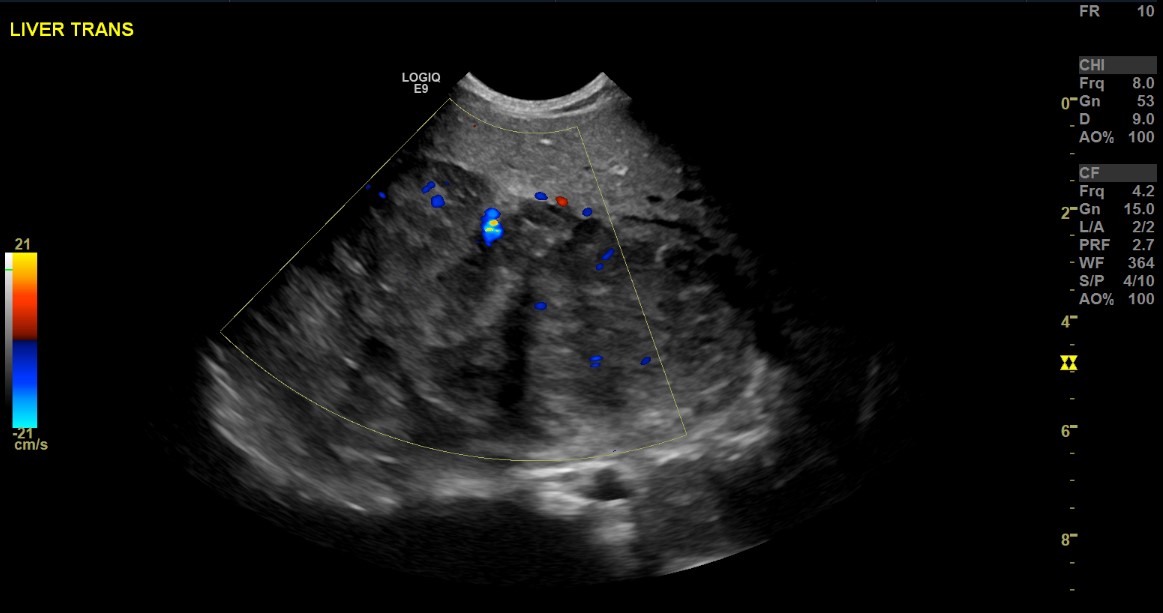
ULTRASOUND ABDOMEN
CONTRAST-ENHANCED CT: ARTERIAL PHASE
CONTRAST-ENHANCED CT: PORTOVENOUS PHASE
Imaging Findings:
[CHEST AND ABDOMINAL RADIOGRAPH]
The supine radiograph of this child demonstrates hepatomegaly, with consequent mass effect and displacement of bowel loops inferiorly and towards the left side. No discrete lung mass or destructive skeletal lesion is identified.
[ULTRASOUND ABDOMEN]
A large well-defined heterogeneous hypoechoic mass is seen at the posterior aspect of the right hepatic lobe, demonstrating intralesional vascularity. This mass is seen distinct from the right kidney. The biliary tree is not dilated.
[CT ABDOMEN]
Cross sectional imaging confirms the presence of a well-defined lobulated heterogeneous arterial-enhancing tumour with washout and central necrosis. No calcifications are seen. Partial encasement of the celiac artery is noted. Compression onto the intrahepatic portion of the inferior vena cava is observed. The middle hepatic vein is not well visualized, which could be due to tumour compression.
[HISTOLOGY FINDINGS]
Histology sections demonstrate fragmented pieces of tumour tissue, formed by trabeculae of hepatoid cells with elevated nuclear to cytoplasmic ratio.
Diagnosis:
Hepatoblastoma. The patient had an alpha-fetoprotein (AFP) level of >200,000 mcg/ml at diagnosis.
Discussion:
Hepatoblastoma is the most common primary hepatic tumour in children and is often diagnosed in the first 3 years of life. The majority of hepatoblastomas are sporadic in nature; however, some are associated with genetic abnormalities and malformations, e.g. Beckwith-Wiedemann syndrome and familial adenomatous polyposis. Prematurity and low birth weight are also reported risk factors for the development of hepatoblastoma. The most common physical finding is the presence of an abdominal mass. The serum AFP level is unanimously the most important clinical marker, which reflects malignant change, response to treatment and relapse.
Hepatocellular carcinoma is a less likely differential diagnosis in this age group, with its peak at approximately 12-14 years and a smaller peak at 2-4 years. It is also more likely to be multifocal than hepatoblastoma, and has an overall worse prognosis.
Radiographic features of hepatoblastoma often include the presence of a right upper quadrant mass or hepatomegaly. On ultrasound, the presence of an intrahepatic heterogeneous but well-defined mass lesion may be identified. Intralesional calcified foci may be visualized as areas of echogenicity with shadowing. Computed tomography findings are consistent with those demonstrated in the featured patient. Classical CT features include a well-defined hypoattenuating heterogeneous hepatic mass with regions of necrosis and/or haemorrhage. Dense calcifications could be seen in up to 40% of cases. Cross-sectional imaging with CT could be useful to evaluate the thorax for presence of pulmonary metastases, which was not present in our patient. Magnetic resonance imaging as an investigative modality could be useful in delineating tumour extent, vascular involvement or lymphadenopathy.
Surgical resection remains as the main treatment of choice. Pre-operative neoadjuvant chemotherapy with the aim of reducing tumour bulk demonstrated excellent treatment response in this patient.