Answer of March 2018
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 40-year-old lady presents with a 3-year history of progressive shortness of breath on exertion, chest discomfort and mild cough. She is afebrile with no prior history of cigarette smoking. Chest radiograph and high resolution CT scan of the thorax were performed for this patient.
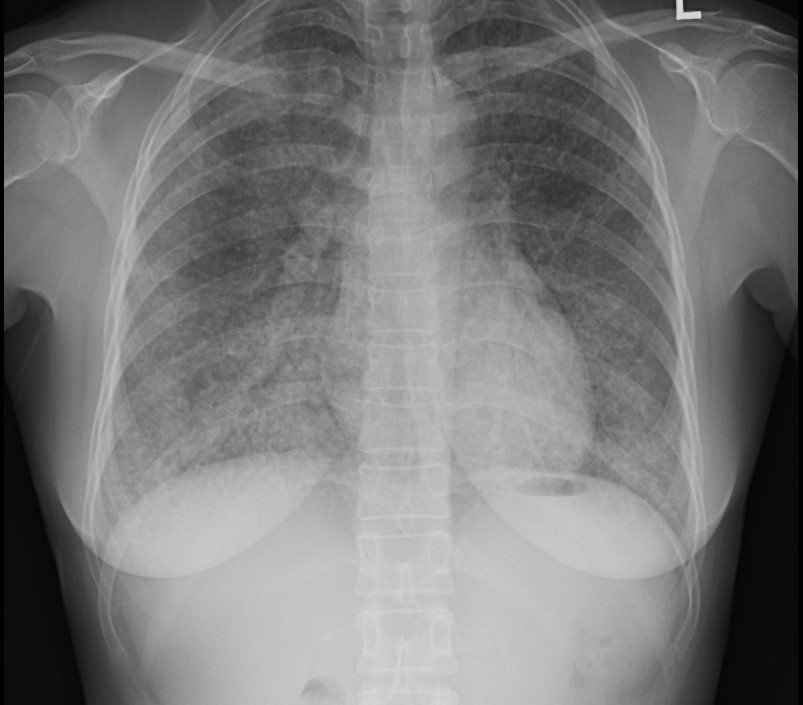
CHEST RADIOGRAPH
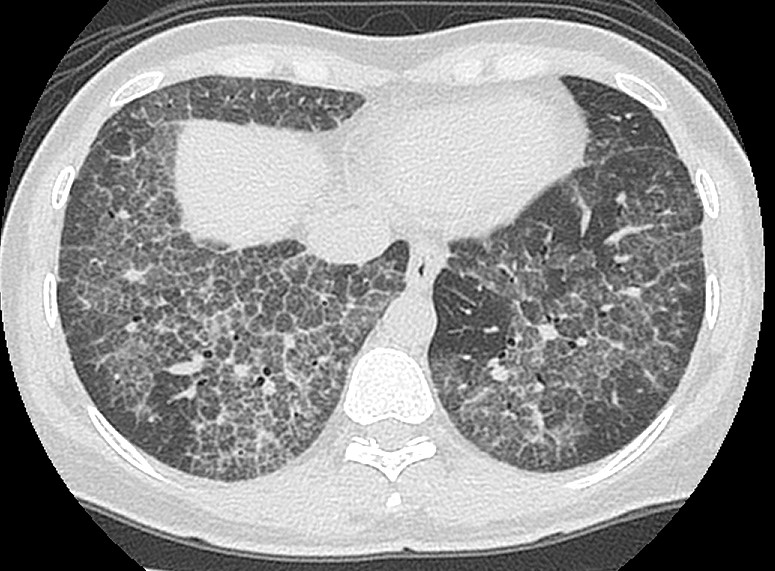
HRCT THORAX
Imaging Findings:
[CHEST RADIOGRAPH]
The erect radiograph of this adult lady demonstrates bilateral, symmetrical reticular densities with central predilection and relative sparing of the apices and costophrenic angles. No focal consolidation is seen. Bilateral lung volumes are preserved. No evidence of pleural effusion is seen. The cardiac shadow is not enlarged.
[HRCT]
Cross-sectional imaging demonstrates smooth thickening of interlobular and intralobular septal lines with the presence of geographic ground-glass opacities. A “crazy-paving” pattern is observed. No evidence of honeycombing or pleural effusion is noted. No significant lymphadenopathy is seen.
[HISTOLOGY: TRANSBRONCHIAL BIOPSY]
Histology sections demonstrate multiple alveoli with amorphous eosinophilic material in the lumina, consisting of type II pneumocytes, lamellar bodies and necrotic alveolar macrophages. No evidence of dysplasia or malignancy is noted.
Diagnosis:
Pulmonary alveolar proteinosis. The patient was subsequently treated with therapeutic whole lung bronchoalveolar lavage.
Discussion:
Pulmonary alveolar proteinosis (PAP) is characterized by abnormal intraalveolar accumulation of surfactant-like material. There is a strong association with cigarette smoking; up to three-quarters of patients are smokers, and in this subgroup, men are 3 times more affected than women. In non-smokers, no specific gender predilection is observed.
Patients with idiopathic PAP experience non-specific respiratory symptoms such as progressive dyspnea (subacute to chronic) with dry cough. Although largely non-specific, the most common elevated serologic marker is lactate dehydrogenase. Granulocyte-macrophage colony stimulating factor may also be raised. Pulmonary spirometry may demonstrate mild to moderate restrictive ventilatory defect, which was present in our patient. Due to macrophage dysfunction or microbial growth medium in the intraalveolar proteinaceous material, these patients are also more susceptible to opportunistic infectious pneumonias.
Differential diagonoses for the chest radiograph appearance could include:
Lymphangioleiomyomatosis (LAM)
Pulmonary Langerhans cell histiocystosis (LCH)
However, this is well differentiated on HRCT findings, which demonstrates greater anatomical detail and extent of the disease. In PAP, a prevalent crazy-paving pattern (smooth thickening of inter and intralobular septae) is observed with geographic ground-glass opacities for PAP. Although “crazy-paving” is deemed as non-specific, central predilection with sparing of apices and costophrenic angles are highly characteristic (but not pathognomonic) for PAP. LAM is a possible diagnosis in this age group and gender; however, the absence of regular, thin walled cysts surrounded by normal lung parenchyma and chylothorax suggests an alternative diagnosis. CT findings of LCH are variable, and often include the presence of irregular nodules and bizarre looking cysts with upper zone predilection and sparing of the costophrenic angles. The diagnosis is also more common in young adult male smokers.
Definitive diagnosis of PAP is typically made at transbronchial / surgical lung biopsy, but specimens obtained from bronchoalveolar lavage (BAL) fluid can also be diagnostic. BAL (whole lung) is considered the main treatment of choice for PAP patients to remove alveolar material.