Answer of February 2018
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
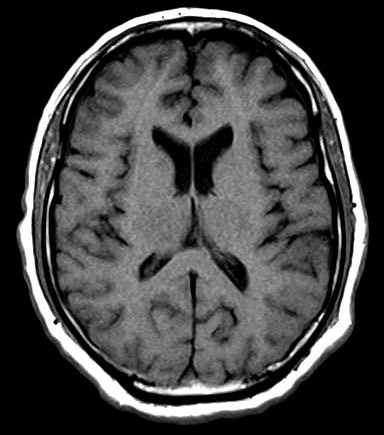
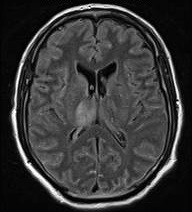
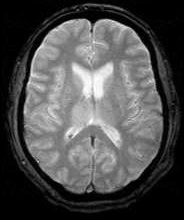
A 59-year-old man who worked as a construction site worked and enjoyed good past health, presented with sudden onset of left lower limb weakness, left upper limb clumsiness, fever, vomiting, confusion and diplopia. Physical examination showed left lower limb power 4/5, with nystagmus, intentional tremor and past-pointing. MRI of the brain was performed.
 |
 |
| Fig. 1: T1W |
Fig. 2: T2W |
 |
 |
| Fig. 3: FLAIR | Fig. 4: DWI |
 |
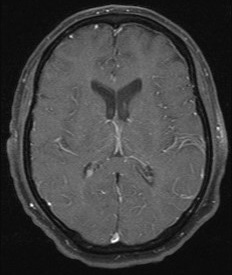 |
| Fig. 5: T2* Gradient Echo | Fig. 6: Contrast-enhanced T1 FS |
Discussion:
Japanese encephalitis (JE) is an acute encephalomyelitis that is a primary viral encephalitis with the vector being a mosquito. At the onset of the disease patients present with severe rigors, fevers and headache. As it progresses to the acute encephalitic stage, meningoencephalitic symptoms such as neck rigidity, cachexia, hemiparesis and convulsions become prevalent.
Most characteristic MRI finding of JE is bilateral T2W thalamic hyperintensity. Unilateral involvement has also been reported but is less common. Other common sites of involvement include basal ganglia, substantia nigra, red nucleus, pons, hippocampus, cerebral cortex, and cerebellum. Subcortical white matter involvement is also reported in some patients, but this has always been in combination with the more characteristic gray matter lesions. Some lesions, especially those in the thalamus, may be hemorrhagic. Enhancement is not usually observed, indicating only minor blood-brain barrier deficit.
There was a significant direct correlation of DWI and ADC values with the disease duration of JE. In acute stage, perivascular cuffing and congestion leading to ischemia and cytotoxic edema results in restricted diffusion and low ADC values.
Bilateral thalamic hemorrhagic lesions identified in JE are also seen in thalamic infarcts due to deep vein thrombosis, occlusion or stenosis of the basilar artery. Other differential diagnosis of bilateral thalamic lesions includes Wernicke’s encephalopathy, Wilson’s disease, acute disseminated encephalomyelitis, systemic lupus erythematous and bithalamic glioma.
JE is treated conservatively as there is no specific antiviral therapy available.