Answer of June 2017
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 37-year-old female patient who enjoyed good past health, presented with sudden onset of headache and vomiting for 1 day. There was no complaint of limb weakness or numbness. Physical examination showed full GCS score with normal hemodynamics. No focal neurological sign was detected. Urgent plain CT brain showed acute intraventricular hemorrhage. CT angiogram of the circle of Willis and DSA cerebral angiogram were subsequently performed.

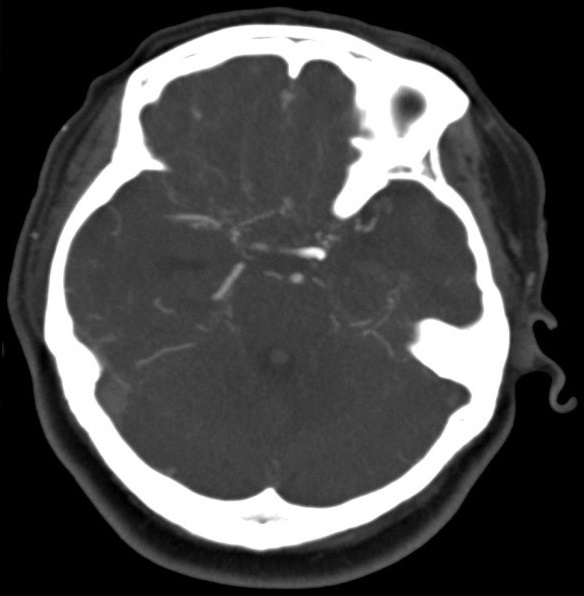
Plain CT Brain
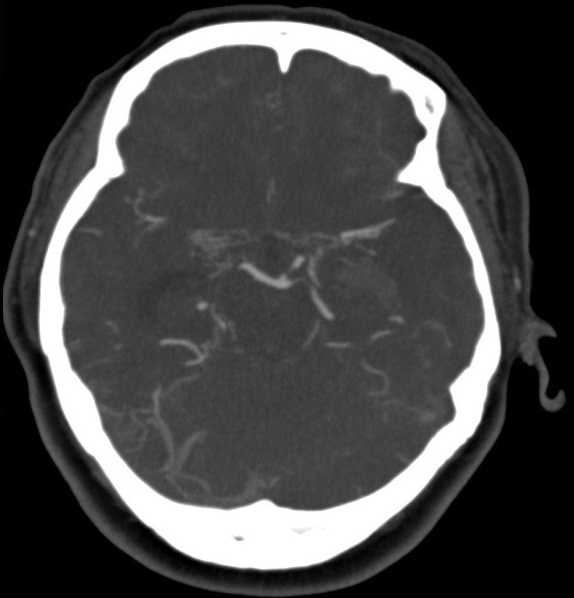
CT angiogram of the Circle of Willis
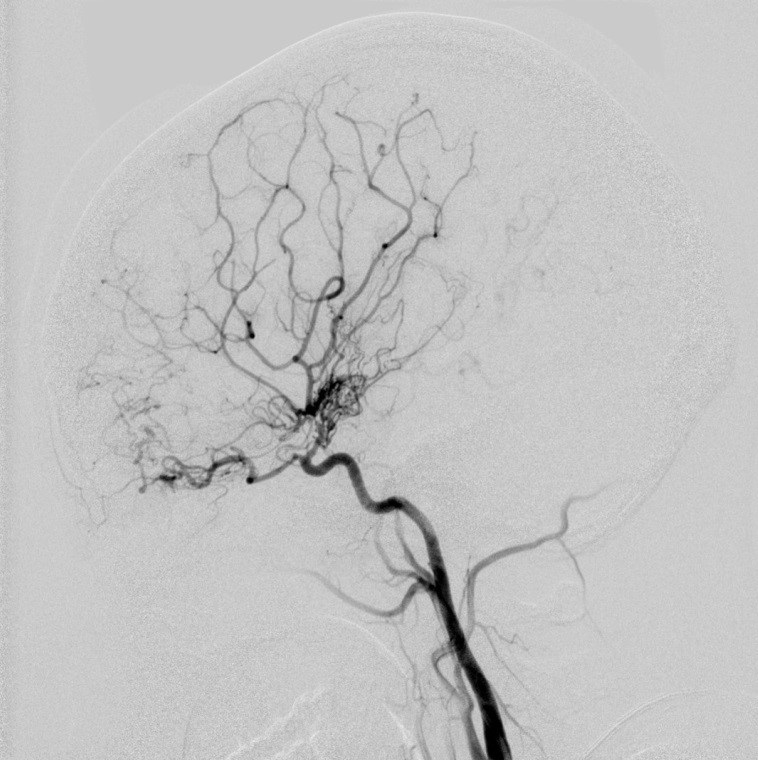
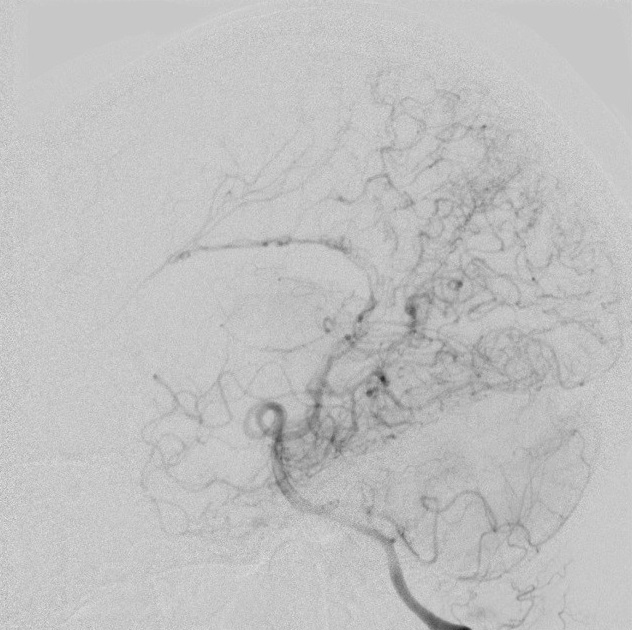
Right ICA DSA lateral projection
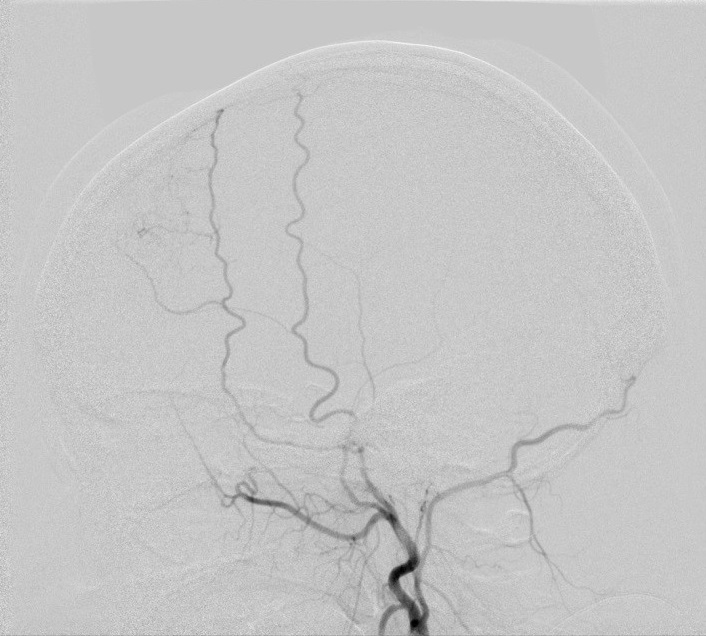
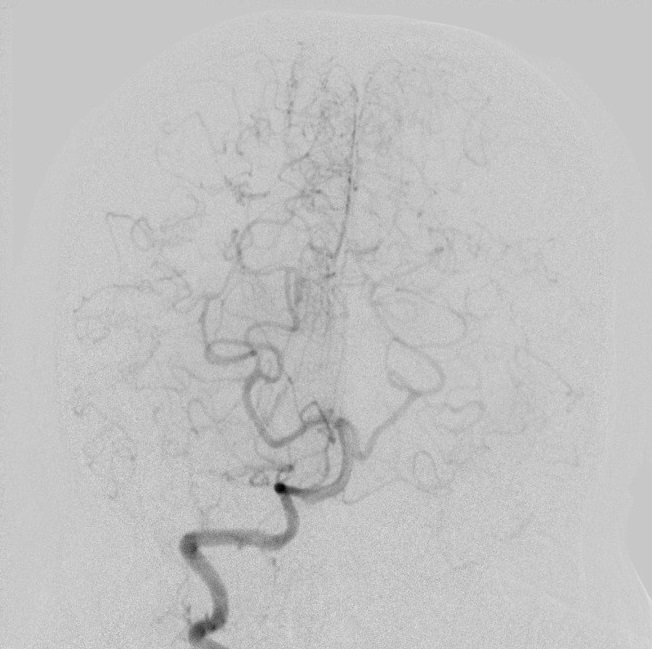
Right ICA DSA PA projection
Right ECA DSA lateral projection
Right ECA DSA PA projection
Right VA DSA lateral projection
Right VA DSA Towne projection
Findings:
CT Brain: Acute intraventricular hemorrhage in bilateral lateral and third ventricles with hydrocephalus
CTA of Circle of Willis: Occluded bilateral terminal ICA, multiple collaterals around the circle of Willis suggestive of puff-of-smoke appearance, markedly attenuated bilateral proximal middle and anterior cerebral arteries.
DSA cerebral angiogram: The terminal right ICA is occluded. The right A1 and M1 are reconstituted by dilated perforators. The distal right ACA territory and part of right MCA territory is reconstituted by PCA branches through pial-pial collaterals. The base of right frontal lobe is supplied by right ophthalmic artery through anastomosis to R ethmoidal arteries. There is transdural synangiosis from right middle meningeal artery supplying part of right frontal lobe. (DSA of the left ICA, ECA, VA showed similar findings, not shown here)
Diagnosis:
Moyamoya disease
Discussion:
Moyamoya disease is an idiopathic, non-inflammatory, non-atherosclerotic progressive vasculo-occlusive disease involving the circle of Willis, typically the supraclinoid internal carotid arteries.
Numerous conditions that can cause arterial occlusion of the circle of Willis, with resultant collaterals, and appearances reminiscent of moyamoya disease. These conditions include neurofibromatosis, tuberous sclerosis, radiation-induced vasculopathy, Down syndrome, atherosclerosis, systemic lupus erythematosus. The term moyamoya disease, is reserved for the idiopathic disease, without any other associated condition. The aetiology of moyamoya disease is poorly understood. Genetic background is frequently mentioned because in 15% of cases, the disease is found in other family members.
The incidence of moyamoya disease is higher in Asian countries, e.g. Japan; in Europe and North America, the prevalence of the disease is considerably lower. The disease is most common in children and young adolescents. There are observed two peaks of incidence – in the first and 3–4 decade of life. The disease is more frequent in women, and the ratio of women to men with the disease amounts to 1.8:1.
Presentation is to some degree age dependent. In children, hemispheric ischemic strokes are most pronounced, whereas in adults, hemorrhage from the abnormal vessels is more common.
CT studies demonstrate non-specific findings resultant from ischemia, such as parenchymal low-density spots, brain atrophy and ventricular dilatation. Hemorrhage may be seen in acute setting.
CT angiography can demonstrate the abnormal net-like vessels in the basal ganglia and at base of brain, giving the characteristic "puff-of-smoke" appearance.
MR imaging can reveal stenosis or occlusion of the distal internal carotid artery and moyamoya vessels, with signal voids in the basal ganglia, as well as ischemia, infarction, atrophy and
ventriculomegaly. Pial collaterals from less affected vessels (especially PCA) forms the so-called ivy sign (high serpentine sulcal FLAIR signal intensity due to slow flow and also high signal on T1 post contrast enhanced MRI).
Characteristic angiographic findings include occlusion or stenosis of the supraclinoid
portion of the ICA and extensive parenchymal, transdural, and leptomeningeal collateral
vessels supplying the ischemic brain.
Bypassing the occlusive segments is the aim of most surgical therapy. In adults, direct revascularization involving external carotid artery to middle cerebral artery (ECA-MCA) anastomoses can be performed as the vessels are larger. One of the surgical options is superficial temporal artery to middle cerebral artery (STA-MCA) bypass. Encephaloduroarteriosynangiosis is the treatment of choice in paediatric patients as their vessels are too small to allow direct anastomosis. This indirect synangiosis involves the placement of the superficial temporal artery onto the brain surface without making a direct connection, in order to promote neoangiogenesis.