Answer of April 2017
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 63-year-old gentlemen with a chronic condition presented with progressive lower limb numbness and constipation for 2 years. Physical examination revealed lower limb hyporeflexia and decreased light touch sensation at left L4 to S1, right L3. MRI was performed.
Figure 1. Sagittal T2W images
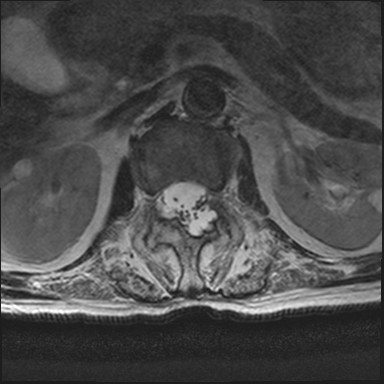
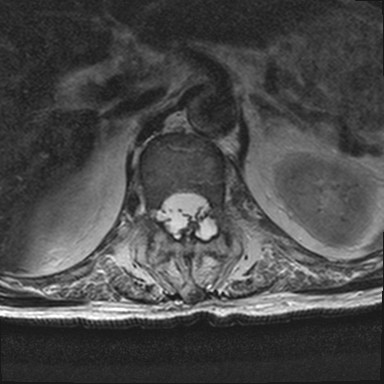
Figure 2. Axial T2W images
Diagnosis:
Dorsal dural diverticula and arachnoiditis from chronic ankylosing spondylitis presenting as cauda equina syndrome
Discussion:
The MR images show features consistent with ankylosing spondylitis, namely vertebral body squaring, bridging syndesmophytes, and fusion of anterior aspects of vertebral body with intervening discs. Multiple dorsal dural diverticula are seen with remodelling of posterior elements and dorsal displacement of multiple nerve roots. Some of the nerve roots appear clumped and tethered to the diverticula.
Dorsal dural diverticula and arachnoiditis are known complications in long-standing ankylosing spondyltiis.
In general, acquired dural diverticula are most commonly seen in the lumbosacral region, where the CSF pressure is greatest. It is seen in patients with connective tissue disorders(e.g. Marfans syndrome, Ehlers-Danlos syndrome), neurofibromatosis type 1, but also reported in long-standing ankylosing spondylitis.
In ankylosing spondylitis, it is postulated that the spread of inflammation from paraspinal ligaments to the dural mater weakens the dura and results in adhesion. Compliance and elasticity of thecal sac is reduced, as is its ability to dampen CSF pressure. The paraspinal ligments are predominantly dorsally located, hence the dorsal location of the diverticula and remodelling of the posterior elements. In contrast, dural ectasia or diverticula from the former causes also involve ventral thecal sac with characteristic posterior vertebral body scalloping.
Cauda equina syndrome in ankylosing spondylitis was first reported by Bowie, Glasgow, and Hauge in 1961. Several etiolgies were proposed, including small vessel angiits of vasa vasorum of nerve roots, nerve root injury from dural ectasia with increased transmitted force from arterial pulsation, as well as arachnoiditis. They remained speculative and none of which gained universal acceptance.
There is yet no effective medical therapy. A meta-analysis found no use in steroid, while NSAID can reduce back pain but not neurology. Lumbroperitoneal shunting, laminectomy or dethering of cauda adhesions were also tried in selected cases with varying success.