Answer of March 2017
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 27 year old lady presented to A&E with acute shortness of breath and left sided pleuritic chest pain for 1 day. She enjoyed good past health and had recently returned from a 2-week trip in Tibet. On admission, her SaO2 was 97% on 2L oxygen and ECG showed sinus tachycardia (about 110bpm). Un-enhanced and contrast-enhanced computed tomography (CT) of thorax was performed as urgent request to exclude pulmonary embolism.
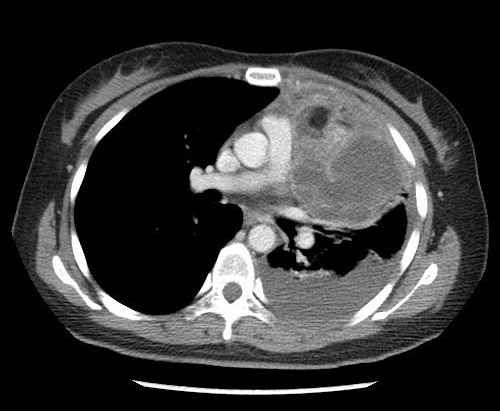
Figure 1. Axial unenhanced CT thorax
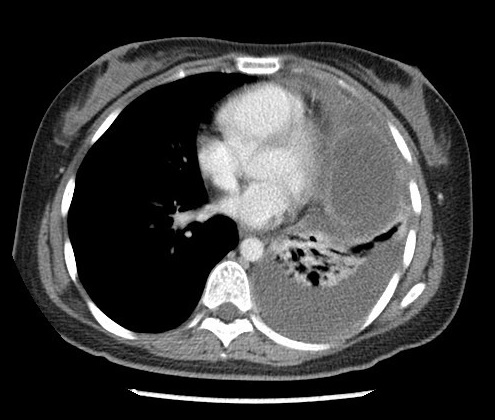
Figure 2. Axial post contrast CT thorax
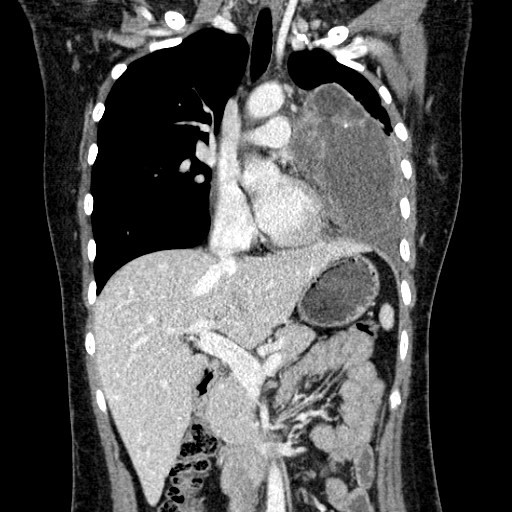
Figure 3. Axial post contrast CT thorax
Figure 4. Axial post contrast CT thorax
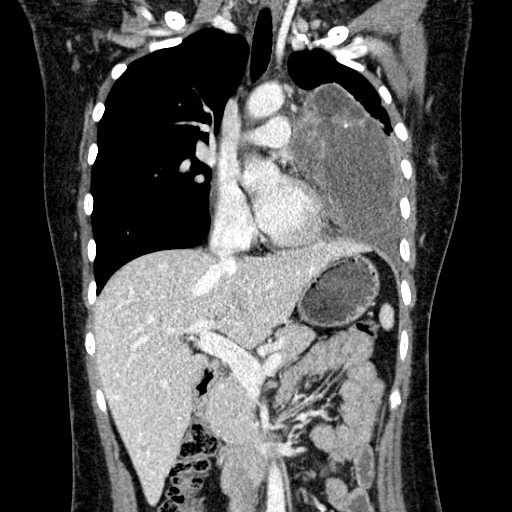
Figure 5. Coronal post contrast CT thorax
Figure 6. Coronal post contrast CT thorax
Diagnosis:
Mediastinal teratoma complicated with rupture into left pleural cavity.
Imaging Findings:
A large multi-loculated cystic mass with macroscopic fat component, enhancing internal septae and a small enhancing solid component is present at anterior mediastinum and left paracardiac region. Curvilinear calcification is detected on unenhanced scan. Postero-inferior wall of the mass is indistinct with associated adjacent moderate left pleural effusion. No macroscopic fat detected within effusion.
Discussion:
Rupture of mediastinal teratoma is an infrequent complication, occurring in up to 36% of cases, most frequently into lung and the tracheobronchial tree, followed by pleura, pericardium, and great vessels. Patients may present with hemoptysis, chest pain, or expectorate hair or sebaceous material.
Among the various hypotheses proposed to explain the possible mechanisms of rupture, the most commonly accepted theory is autolysis of the walls of the tumor by the digestive enzymes produced by tissues (pancreas, intestine, salivary gland) leading to rupture. Malignant teratoma are not prone to rupture as they are predominately solid and they are less likely to contain well differentiated tissue such as pancreatic cells.
Radiological signs of rupture depend on the space into which rupture occurs. Rupture into lung parenchyma can cause chemical pneumonia and occasional abscesses. Rupture into pleural or pericardial space may result in effusions. Fat fluid level in pleural effusion has been reported and considered pathognomonic. Effusions may be caused by a direct spillage of internal components of the tumor or a pleural! pericardial inflammatory reaction to extravasated tumor contents.
Differentiation between ruptured benign mediastinal teratoma and malignant teratoma with pleural invasion may sometimes be difficult. CT findings of predominate solid component, spiculated border or direct invasion into surrounding organs are more suggestive of malignant teratoma. A history of sudden onset of symptoms is also a helpful clue towards diagnosing ruptured teratoma.
Surgical excision is definitive treatment for ruptured mediatstinal teratoma and the prognosis is good. However, inflammation and secondary adhesion in lung or pleural cavity may render the process particularly challenging. Often adjacent thymus, pericardium and lung may have to be resected due to the teratoma’s firm adherence. Delayed surgery will increase difficulty for complete resection.