Answer of February 2017
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 68 year old lady with history of left hemithyroidectomy for non-toxic multinodular goiter was found to have a suspicious left-sided neck lesion detected on ultrasound in the surgical follow up clinic. She was referred for ultrasound guided fine needle aspiration. A targeted ultrasound, contrast MRI and CT neck were performed.
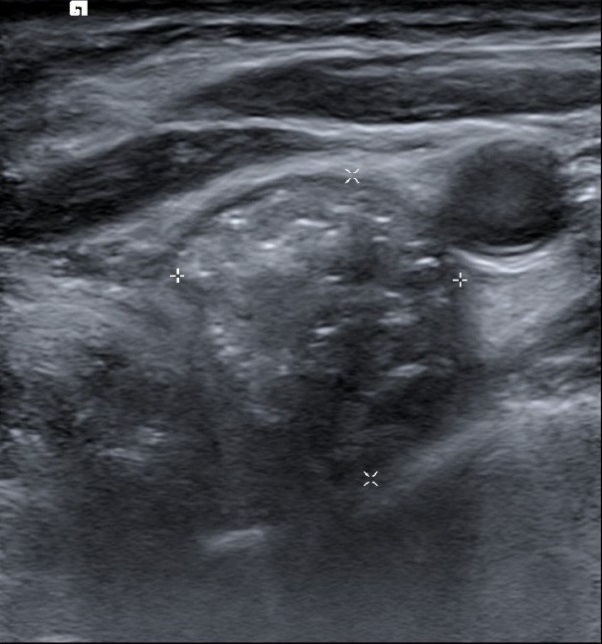
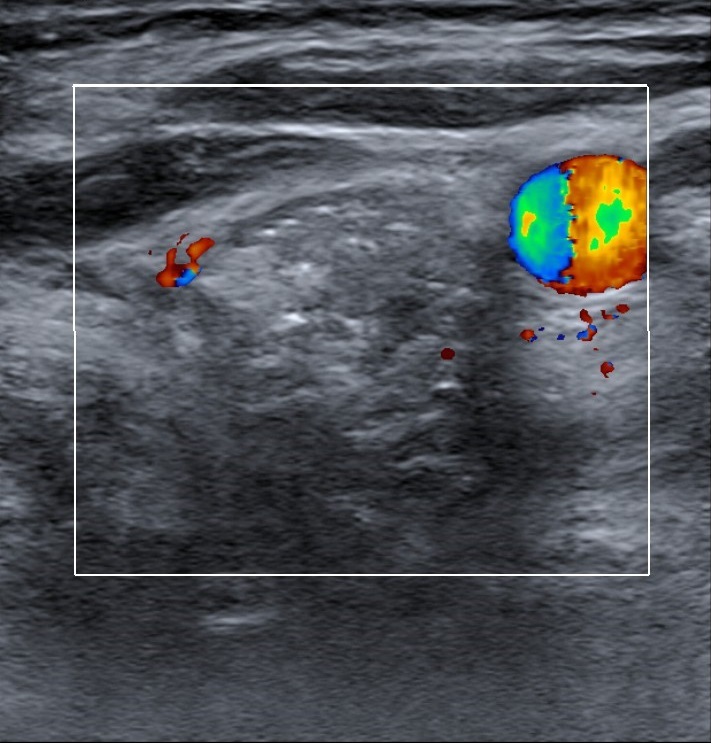
Figure 1. US
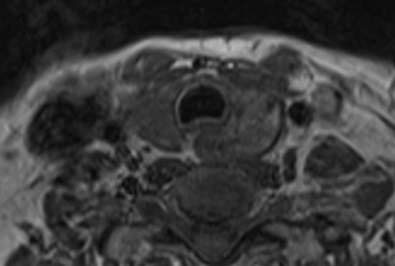
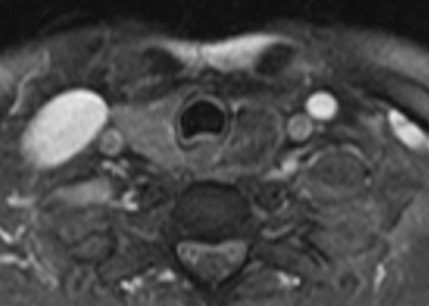
Figure 2. MRI (T1, T2, Post-Gd T1 FS axial)
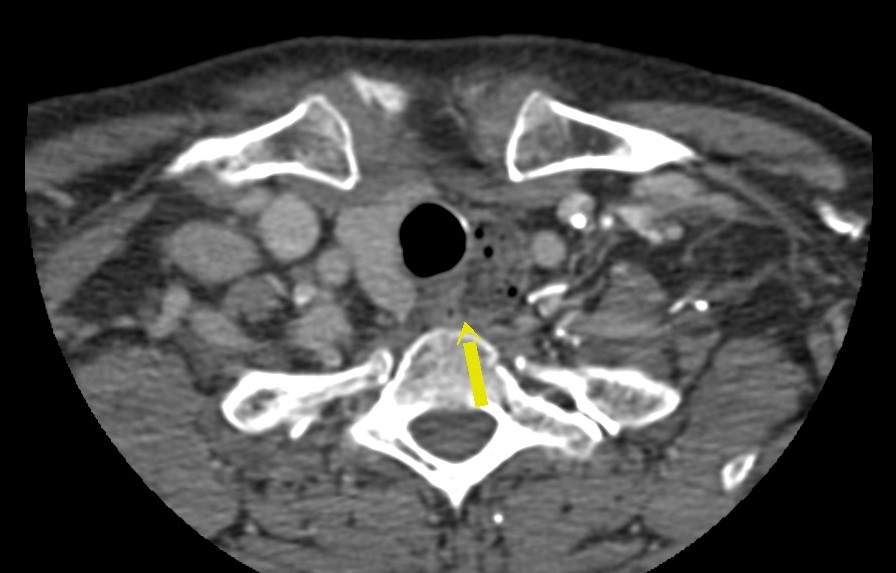
Figure 3. CT
Killian-Jamieson diverticulum
Discussion:
The targeted ultrasound of the left neck lesion showed a well-circumscribed heterogeneous echogenic lesion over the left thyroid bed between the trachea and left common carotid artery. It showed posterior acoustic shadowing with no intralesional Doppler signal detected.
On contrast CT neck, the lesion was found to be originating from the left anterolateral wall of the cervical esophagus just below the level of cricoid cartilage, containing mottled densities. It was also confirmed on the contrast MRI, which showed T1W and T2W mildly heterogenous hyperintense signal with peripheral mucosal enhancement. Supplementary barium swallow was also performed, showing a persistent contrast-filling outpouching from the left lateral wall of upper esophagus. Overall findings are consistent with a Killian-Jamieson diverticulum.
Killian-Jamieson diverticulum is a rare form of cervical esophageal diverticulum, which is distinct from the more commonly known Zenker’s diverticulum. It is a pulsion-type of diverticulum which protrudes through the Killian-Jamieson space, and can be transient or persistent. The KJ space is a muscular gap over the anterolateral wall of the esophagus, through which the inferior laryngeal nerve passes and enters the pharynx. It is bounded anteriorly by the cricoid cartilage, superolaterally by the cricopharyngeus muscle and inferomedially by the longitudinal tendon of the esophagus, where it inserts on to the cricoid cartilage. The majority of KJ diverticula is small in size (<1.5cm), unilateral (75%) and left-sided.
Most patients with KJ diverticulum are asymptomatic. For the symptomatic patients, they usually present in the seventh to eighth decades, with the most common symptom being oropharyngeal dysphagia. Retention of food material in the diverticulum can also result in regurgitation, halitosis, chronic cough, or even aspiration. Rarely, complications may arise, such as ulceration, hemorrhage, tracheoesophageal fistula and squamous cell carcinoma.
Barium swallow or esophagography is usually the preferred initial examination for KJ diverticulum, which may be seen as a smooth contrast-containing outpouching arising from the anterolateral wall of cervical esophagus. Food debris, if present, may be seen as filling defects within the outpouching. The relationship of the diverticula opening with the cricopharyngeus muscle can also be assessed during the passage of barium bolus, which outlines the cricopharyngeal bar, which represents the constriction of cricopharyngeal muscle. In addition, abnormal pharyngoesophageal motility may also be assessed on fluoroscopic study.
The anatomical relationship of the diverticular sac with the adjacent structures may be further assessed by contrast CT of the neck region. KJ diverticulum appears as a well-defined outpouching arising from the lateral wall of cervical esophagus, containing gas and mottled densities, which represent presence of food debris. The larger ones may cause mass effect with displacement and/ or compression on the adjacent trachea, thyroid and other soft tissues. Complications such as development of squamous cell carcinoma can also be detected on CT.
Zenker’s diverticulum is an important differential for KJ diverticulum. Despite their common origin near the cricopharyngeus, these two types of diverticula are anatomically distinct. Zenker’s diverticulum originates from the posterior wall of the cervical esophagus in the midline just above the cricopharyngeus (i.e., Killian's dehiscence), whereas KJ diverticulum originates from the anterolateral esophageal wall at the KJ space as previously described. In addition, Zenker’s diverticulum is usually larger in size and is more commonly symptomatic.
KJ diverticulum is usually managed conservatively. In symptomatic cases or those with large KJ diverticula, endoscopic or surgical treatment including diverticulotomy and diverticulopexy may be considered.