Answer of September 2016
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
Figure 1. Orthopantomogram

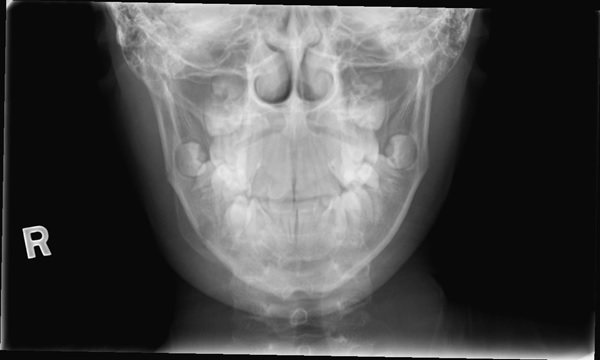
Figure 2. Frontal Radiograph
Figure 3. Lateral Radiograph
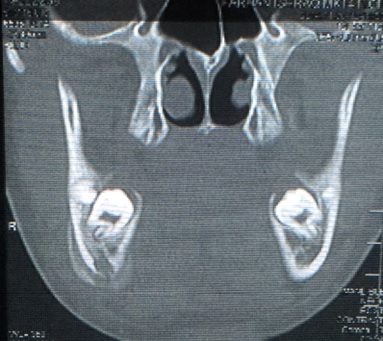
Figure 4. Coronal CT Image
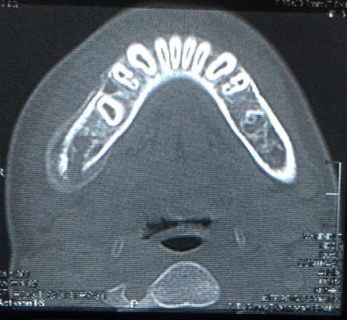
Figure 5. Axial CT Image
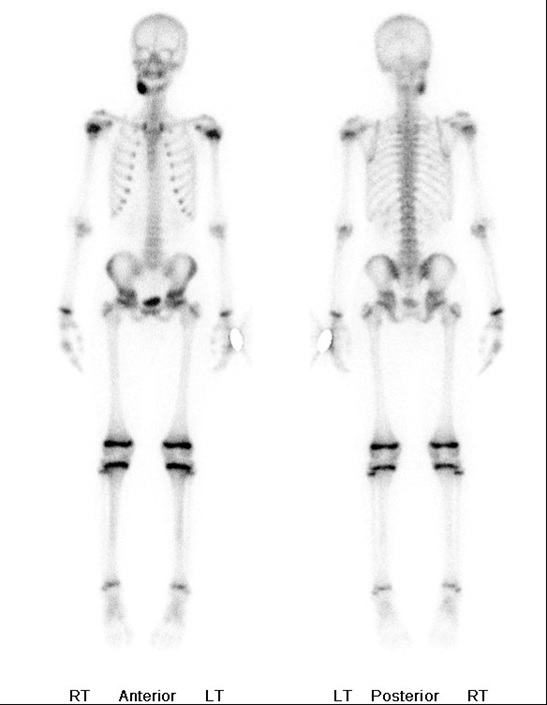
Figure 6. Bone Scintigraphy
Diagnosis:
Chronic osteomyelitis.
Garre’s sclerosing (non-suppurative) osteomyelitis.
Discussion:
Plain radiograph revealed an osteolytic lesion at the body and angle of right mandible, with smooth solid periosteal thickening and peripheral reactive bone formation. It was not associated with an unerupted tooth. Computed tomography showed a lucent lesion and laminated bone deposition at the inferior cortex of the mandible, with a small cortical break. There was relatively little bone destruction. Bone scintigraphy showed corresponding increased tracer uptake at right mandible. No other abnormal uptake was seen in the rest of skeleton.
The patient subsequently underwent a biopsy of the lesion. Gross buccal expansion was noted macroscopically. The lesion was chalky in consistency. No pus discharge was seen. Pathology revealed reactive bone formation, consistent with osteomyelitis. Ziehl-Neelsen and Gram stains fail to demonstrate micro-organisms in the specimen
The underlying causative infective agent was later found as dental examination showed carious right lower 1st molar tooth. The causal infected tooth was extracted with subsequent improvement of patient’s symptoms. Radiograph taken 5 months later showed resolution of the lesion.
The clinical manifestations, radiological findings and disease course in this case were classical of Garre’s sclerosing osteomyelitis.
The disease was first described by C Garre in 1893. It is also known as chronic non-suppurative osteomyelitis with proliferative periostitis. It is a distinct entity of chronic osteomyelitis seen exclusively in children and young adults, as a result of chronic irritations or mild infections, most notably dental caries. It is unique in its tendency to cause thickening of bone with periostitis, without development of suppuration and fistula formation. White cell count and Inflammatory markers such as C-reactive protein are frequently not elevated. In fact, most patients experience relatively little pain, and it is the facial asymmetry that brings the patients to seek treatment.
Mandible is the most commonly affected region, followed by maxilla. Reactive periosteal thickening can be marked, and may be radiologically alarming and worrisome for underlying bone malignancy. Differential diagnoses should include osteoblastic osterosarcoma and Ewing’s sarcoma in this age group. These malignancies may also show laminated periosteal reaction but usually have a more aggressive growth pattern. In Ewing’s sarcoma, significant soft tissue involvement is usually present.
For the majority of patients, an underlying source of infection, usually longstanding dental caries, can be found. The removal of underlying irritants typically results in resolution of the periostitis.