Answer of May 2016
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 57-year-old gentleman with history of hypertension has a routine chest radiograph. He is completely free of any chest symptom. Chest radiograph and subsequent high-resolution CT thorax taken two weeks later were available.
Chest X-Ray
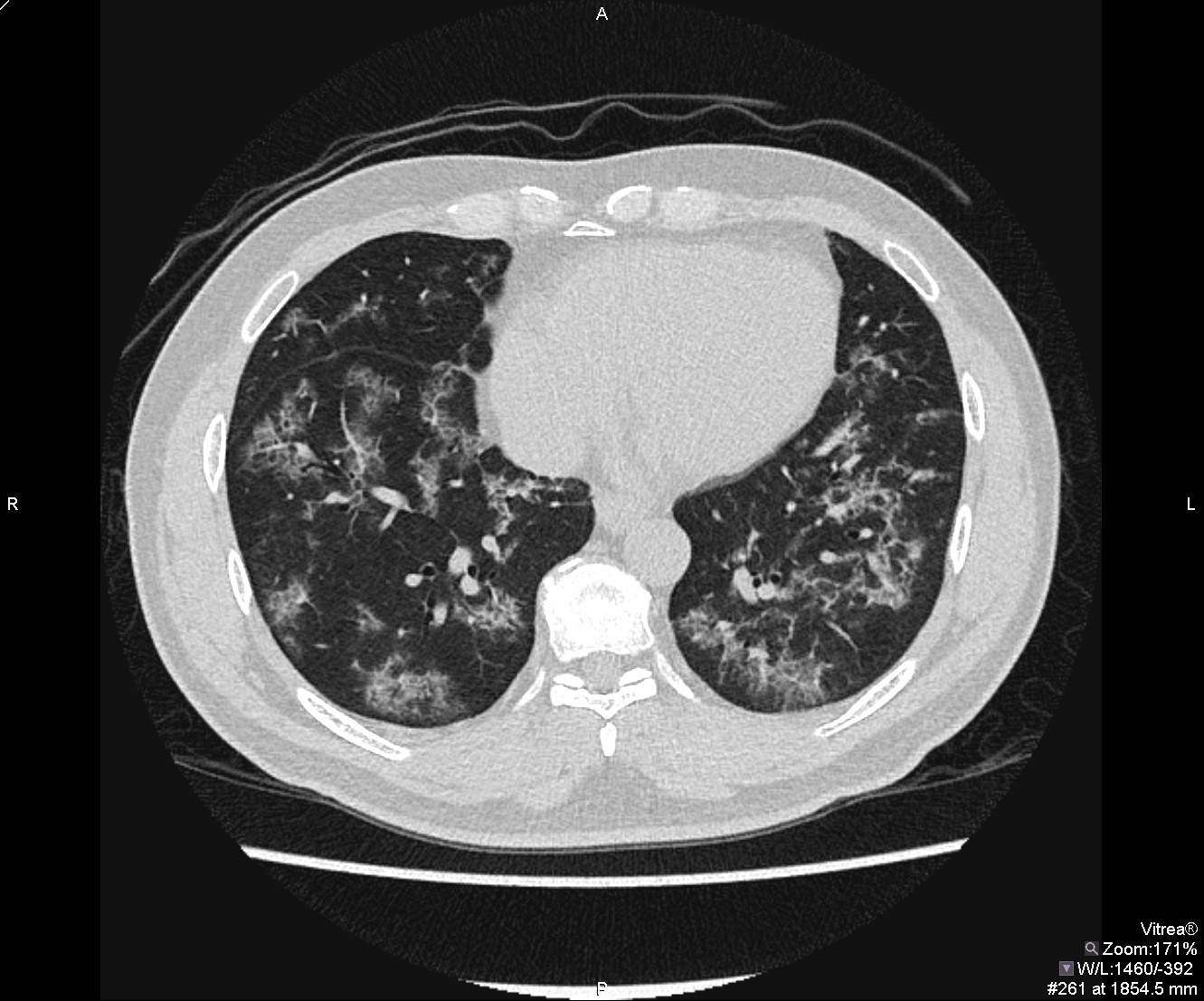
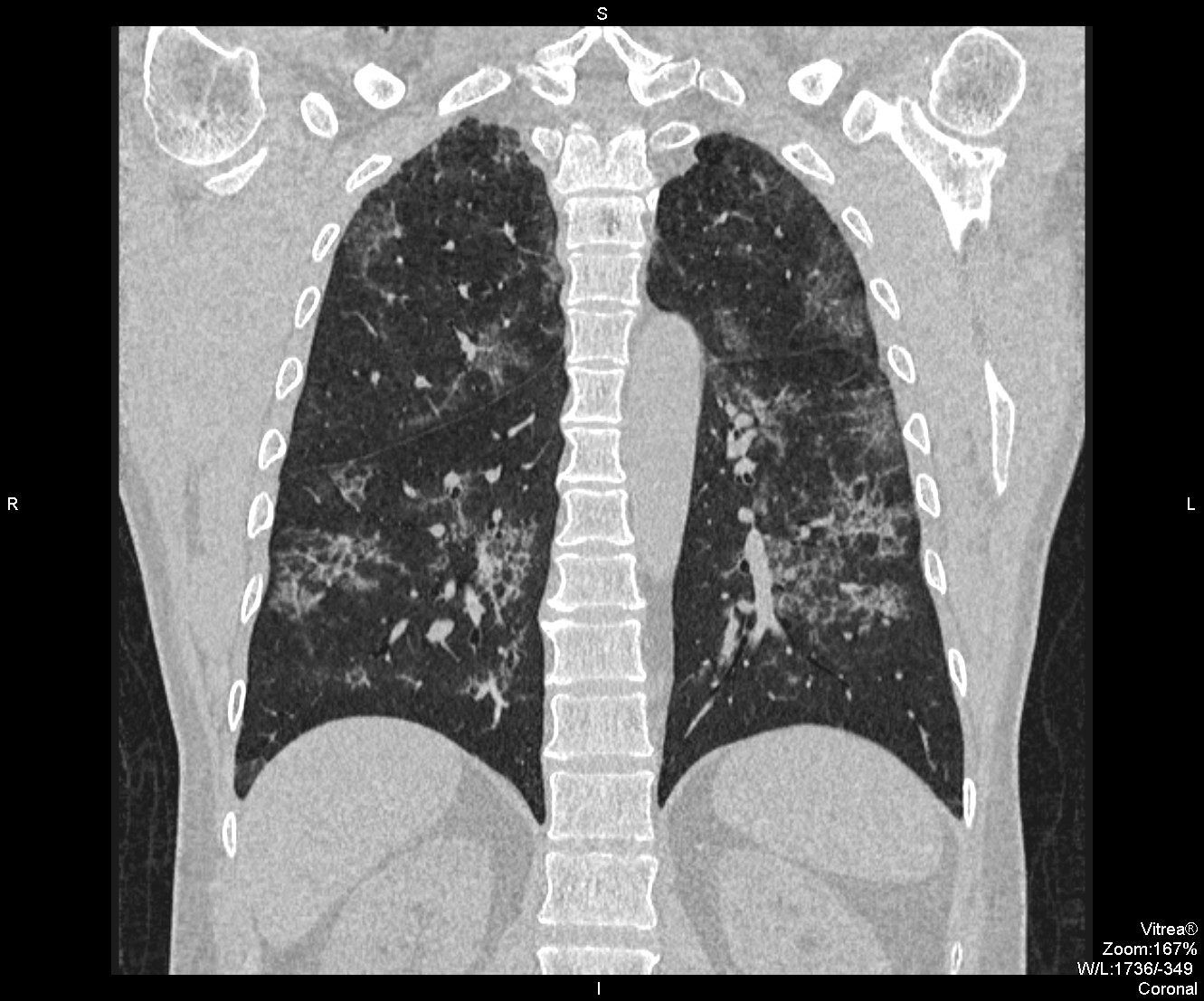
High Resolution CT Thorax
Diagnosis:
Pulmonary Alveolar Proteinosis (PAP)
Discussion:
Initial chest x-ray revealed bilateral airspace consolidation predominately in the perihilar regions. High resolution CT thorax demonstrates patchy ground glass opacities and superimposed smoothly thickened septal lines, giving a ‘crazy-paving’ pattern. These changes are located centrally and symmetrically, demonstrate sharp demarcation with normal lung, and show relatively sparing of the costophrenic angles, basilar subpleural zones and lung apices. The striking difference between the lack of clinical symptom and the grossly abnormal radiological appearance supports a diagnosis of pulmonary alveolar proteinosis. Patient was subsequently referred for bronchoscopy examination which shows a milky aspirate. Histology from transbronchial biopsy confirmed the presence of material within alveoli which is stained positive with Papanicolaou and periodic acid-Schiff (PAS).
Pulmonary alveolar proteinosis is a rare lung disease that is related to altered homeostasis of pulmonary surfactants and is characterized by pathological alveolar accumulation of surfactants.
Patients suffering from pulmonary alveolar proteinosis can be asymptomatic in up to 20% of cases. Patients may also experience nonspecific, moderate respiratory symptoms including progressive dyspnea, and dry or minimally productive cough. Less common signs and symptoms include fatigue, weight loss, low-grade fever, chest pain, and hemoptysis. Physical examination may reveal crackles, clubbing or cyanosis.
The most common elevated serological marker for PAP is elevated lactate dehydrogenase level, but this finding is nonspecific.
Radiographic features of pulmonary PAP include bilateral central airspace opacities with relative sparing of the apices and costophrenic angles. Opacities can range from ground glass appearance with ill-defined margins, to reticular or reticulonodular, to consolidation with air bronchogram. There is typically no adenopathy, cardiomegaly or pleural effusion. There is often notably disparity between the clinical symptomatology and the more extensive radiographic abnormalities.
High-resolution CT thorax typically shows “crazy-paving” appearance, which is the network of smoothly thickened interlobular septal lines superimposed on area of ground glass opacities. There is typically a sharp demarcation between normal and abnormal lung. Of importance, this CT appearance alone is non-specific. Differential diagnosis is wide and can include adult respiratory distress syndrome, pulmonary haemorrhage syndromes, neoplastic cause such as bronchoalveolar carcinoma (now known as atypical adenomatous hyperplasia-adenocarcinoma spectrum), inflammation or infection such as pneumocystis pneumonia, lipoid pneumonia, organizing pneumonia or non-specific interstitial pneumonia.
Definitive diagnosis is made with lung biopsy or bronchoalveolar lavage specimens that reveal intraalveolar deposits of proteinaceous material, dissolved cholesterol and eosinophilic globules that is PAS stain positive. Symptomatic treatment includes whole-lung lavage, and multiple procedures may be required.